Antimicrobial Resistance
FDA's role in antimicrobial resistance (AMR) preparedness and response, and information about AMR
On this page:
What's new | The FDA's role and strategic approach | Product development | Antimicrobial stewardship | Surveillance and monitoring | Regulatory science | FDA publications | Information for consumers | Press and statements | Events | Interagency collaboration | Contact the FDA
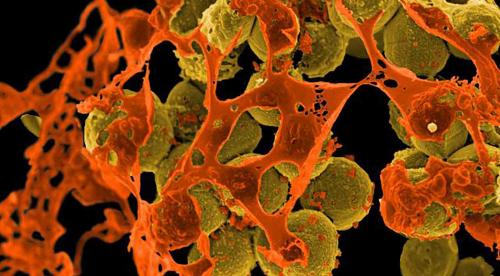
Antimicrobial resistance (AMR)—the ability of a microorganism (bacteria, virus, fungi, parasite) to resist the effects of a drug—is a serious, complex and costly public health problem.
According to the Centers for Disease Control and Prevention, each year in the United States at least 2.8 million antibiotic-resistant infections occur, and more than 35,000 people die as a result. Combating AMR requires multifaceted efforts in both the healthcare and veterinary sectors.
What's new
- February 12, 2026: The FDA has finalized GFI #273: Defining Durations of Use for Approved Medically Important Antimicrobial Drugs Fed to Food-Producing Animals. This guidance provides recommendations on how animal drug sponsors may voluntarily establish defined durations of use for a subset of approved medically important antimicrobial drugs that are approved for use in food-producing animals and currently lack a defined duration of use.
- January 8, 2025: The FDA released a request for comments (RFC) soliciting public input on new opportunities and emergent monitoring needs for possible inclusion in the forthcoming National Antimicrobial Resistance Monitoring System (NARMS) 2026-2030 Strategic Plan. The Federal Register notice about the RFC includes instructions for submitting comments, as well as specific questions and requests for information meant to prompt helpful submissions. The 75-day comment period will be open from January 10 to March 26, 2025.
- November 18, 2024: New consumer article and video now available! Learn how you can safely use antibiotics so you can get well, protect yourself and your family, and combat antimicrobial resistance.
- October 10, 2024: The FDA announced the publication of the 2023 Summary Report on Antimicrobials Sold or Distributed for Use in Food-Producing Animals. The 2023 data indicate that U.S. sales and distribution of medically important antimicrobial drugs approved for use in food-producing animals decreased by 2% between 2022 and 2023; this represents a 37% decrease in sales since the sales peaked in 2015.
- October 9, 2024: The U.S. Environmental Protection Agency (EPA) finalized its framework for expanding federal collaboration on the review of antibacterial and antifungal pesticides. In developing the framework, EPA coordinated with the U.S. Department of Health and Human Services (HHS) and the U.S. Department of Agriculture (USDA), under the oversight of the White House Office of Science and Technology Policy. The framework establishes a process for EPA to consider input from the other federal agencies on whether use of antibacterial or antifungal pesticides might reduce the effectiveness of some human and animal antibacterial and antifungal drugs.
The FDA's role and strategic approach
Antimicrobial resistance is recognized as a growing global threat. In 2014, the White House announced the National Strategy for Combating Antibiotic-Resistant Bacteria (CARB), underscoring the need for a coordinated inter-agency response to this threat. The FDA has been and continues to be integral in these efforts.
Several of FDA’s Centers—including the Center for Drug Evaluation and Research (CDER), Center for Devices and Radiological Health (CDRH), Center for Biologics Evaluation and Research (CBER), Center for Veterinary Medicine (CVM), National Center for Toxicological Research (NCTR), and the Office of the Chief Scientist—play key roles in combating AMR.
The FDA is dedicated to addressing the challenges AMR presents by helping to preserve the effectiveness of currently available antimicrobial drugs and promoting the development of new medical products that can help reduce the emergence and spread of AMR bacteria.
Working with both domestic and international partners, the FDA is proactively addressing the complex challenges associated with the growing threat of AMR by:
- Facilitating efficient product development to address AMR, including the development of new antimicrobials, diagnostic tests, and vaccines
- Promoting the appropriate and responsible use of antimicrobials and disseminating information promoting interventions that help slow the development of resistance
- Supporting the development and enhancement of tools for conducting surveillance of antimicrobial use and resistance so stakeholders can better track, treat, or respond to AMR outbreaks
- Advancing regulatory science to develop the tools, standards, and approaches to facilitate the translation of breakthrough discoveries in science and technology into innovative, safe, and effective medical products
To achieve this mission, the FDA will continue to work collaboratively with Congress, its partners at other U.S. government agencies, and other stakeholders to find additional ways to prevent, detect, and address AMR.
Product development
The FDA works closely with product sponsors and other government agencies to facilitate efficient product development to address AMR, including new antimicrobial drugs, biologics (including human vaccines), and diagnostics.
- The FDA employs a variety of mechanisms, where appropriate, to help speed the development and availability of medical products for humans: Fast track designation, priority review, and breakthrough therapy designation.
- Under Generating Antibiotic Incentives Now (Report to Congress; PDF, 545 KB), or GAIN, the FDA is authorized to provide a five-year extension of exclusivity to incentivize the development of new Qualified infectious disease products (QIDPs) (PDF, 390 KB). A QIDP is defined as “an antibacterial or antifungal drug for human use intended to treat serious or life-threatening infections, including those caused by an antibacterial or antifungal resistant pathogen.” As of August 2018, the FDA has approved 15 new QIDPs for bacterial or fungal infections.
- Established by Congress under the 21st Century Cures Act, the Limited Population Pathway for Antibacterial and Antifungal Drugs, or LPAD pathway, is a new step to help advance development of antimicrobial drugs for limited populations of patients with unmet need.
- The FDA is also in discussion with other agencies including the Centers for Medicare and Medicaid Services (CMS) to explore the means for reimbursement of certain new antibacterial drugs that meet critical patient and public health needs.
The FDA is working to advance the development of nontraditional antimicrobial products including:
- Bacteriophages (viruses that infect, replicate within, and ultimately destroy bacteria)
- Live biotherapeutic products (LBP) (biological products that 1) contain live organisms, such as bacteria; 2) are applicable to the prevention, treatment, or cure of a disease or condition of human beings; and 3) are not a vaccine)
- Also see from CBER: Early Clinical Trials with Live Biotherapeutic Products: Chemistry, Manufacturing, and Control Information (Guidance for Industry) (PDF, 174 KB)
- Microbiome therapies (e.g., fecal microbiota for transplantation (FMT))
- Also see from CBER: Regulatory Considerations for Fecal Microbiota Transplantation Products. Cell Host &Microbe 27:173-175, 2020; DOI 10.1016/j.chom.2020.01.018
- Immune-modulators
The FDA is also working to advance the development of vaccines for organisms contributing to AMR.
- Also see from CBER: General Principles for the Development of Vaccines to Protect Against Global Infectious Diseases (Guidance for Industry) (PDF, 58 KB)
The FDA encourages the development of novel in vitro diagnostic (IVD) devices for detection of AMR associated with microbial pathogens. Also see: Antimicrobial Susceptibility Testing - Helping Health Care Providers Determine the Appropriate Antimicrobial Agent for Treatment
When searching for AMR-related device approvals it is helpful to know the associated Product Code for the class of AMR-related devices.
- You can find these codes in the CDRH Product Classification database, by searching for the terms susceptibility, antimicrobial, or resistance in the “device” section.
- While not a complete list, examples of Product Codes associated with AMR-related device approvals include: JTN, JWY, LON, LTT, LRG, LTW, PEN, PAM, and POC.
- These Product Codes include phenotypic antimicrobial susceptibility test (AST) devices and devices that determine AMR by other means, such as genetic markers. (FDA maintains a list of cleared or approved Microbial Nucleic Acid Devices; please note that this list also includes other devices that do not detect genetic markers of resistance.)
- Knowing the Product Code also makes it easier to find specific AMR-related device approvals when searching the PMA, de novo, and 510(k) databases.
April 30, 2024: BioMérieux is recalling VITEK 2 AST cards, an AST kit, due to a higher concentration of ceftriaxone antibiotic in two wells. This kit is used for testing how sensitive bacteria are to antibiotics.
- Recently cleared IVD devices, including Antimicrobial Susceptibility Test (AST) devices, include:
- February 15, 2024: The FDA cleared the PBC [positive blood culture] Separator with Selux Antimicrobial Susceptibility Testing (AST) System from Selux Diagnostics, Inc. to be marketed in the U.S. The PBC Separator with Selux AST System is an automated lab inoculation preparation system intended for use with positive blood culture samples that can be used for quantitative in vitro antimicrobial susceptibility testing without the traditional overnight subculture.
- July 6, 2023: The FDA cleared HardyDisk AST Sulbactam/Durlobactam 10/10μg (SUD20) (K231568), a disk diffusion assay for in vitro susceptibility testing of Sulbactam/Durlobactam, a new drug approved for the treatment of hospital-acquired bacterial pneumonia (HABP) and ventilator-associated bacterial pneumonia (VABP) caused by Acinetobacter baumannii-calcoaceticus complex. This assay was cleared just 6 weeks after new drug approval.
- July 5, 2023: The FDA cleared VITEK 2 AST-Gram Positive Daptomycin (≤0.12 - ≥8 µg/mL) (K230864), a miniaturized, abbreviated and automated version of the classic broth dilution method to determine the minimum inhibitory concentration of daptomycin, an antibiotic with updated breakpoints for testing Enterococcus faecalis. In addition, claims for testing vancomycin-resistant E. faecalis were added due to FDA recognition of breakpoints.
- May 4, 2023: The FDA cleared the BD Kiestra Methicillin-resistant Staphylococcus aureus (MRSA) Application (K213280), an in vitro diagnostic software program for use with the BD Kiestra Laboratory Automation Solution for the qualitative assessment of microbial colonies on chromogenic culture media to aid in the prevention and control of methicillin-resistant Staphylococcus aureus (MRSA) infection.
- April 19, 2023: The FDA cleared the Selux AST System (K211748) for use with the Selux Gram-Negative Comprehensive Panel through the 510(k) premarket notification pathway. This follows clearance (K211759) of the system earlier this year for use with the Selux Gram-Positive Comprehensive Panel. The Selux AST System is an in vitro diagnostic test system used for antimicrobial susceptibility testing. This testing is performed to determine whether an organism is susceptible or resistant to an antimicrobial drug to help physicians select the appropriate drug to treat an infection. The Selux AST System allows for simultaneous testing of a larger number of drugs and drug concentrations than previous systems. The two panels also have the ability to expand to incorporate new drugs in the future. Susceptibility testing systems use FDA-recognized cut-off values (referred to as susceptibility test interpretive criteria or breakpoints), to indicate whether the drug is likely to be effective (drug concentrations below the cut-off are likely to be effective, and drug concentrations above the cut-off are not likely to be effective). Since breakpoints can be updated to maintain clinical success of the drug, the Selux AST System was also cleared with a prospective change protocol, allowing the developer to update breakpoints without an additional premarket submission to the FDA. This is the latest example of the FDA’s ongoing commitment to advance access to safe and effective antimicrobial susceptibility testing intended to aid healthcare professionals in making more informed decisions for patients.
- March 21, 2023: The FDA cleared the Sensititre 20–24-hour Haemophilus influenzae/Streptococcus pneumoniae MIC or Breakpoint Susceptibility System with Delafloxacin in the dilution range of 0.00025-8 µg/ml (Streptococcus pneumoniae) and 0.000125-8 µg/ml (Haemophilus influenzae) (K223844) a miniaturized version of the classic broth dilution method to determine the minimum inhibitory concentration of delafloxacin, an antibiotic approved for the treatment of community-acquired bacterial pneumonia (CABP) and acute bacterial skin and skin structure infections (ABSSSI). Claims were added for testing Streptococcus pneumoniae and Haemophilus influenzae isolates recovered from CABP.
- March 20, 2023: The FDA cleared the Colibri System (K223245), an automated pre-analytical processor that picks isolated colonies to prepare MALDI-TOF MS target slides for bacterial identification and microbial suspensions at a known concentration for antimicrobial susceptibility testing. This system is an updated workflow from the previously cleared semi-automated system.
- March 10, 2023: The FDA cleared the Sensititre YeastOne Susceptibility System with Fluconazole in the dilution range of 0.12-128 μg/mL (K221198), a miniaturized version of the classic broth dilution method to determine the minimum inhibitory concentration of fluconazole, an antifungal agent with updated breakpoints for testing C. albicans, C. glabrata, and C. parapsilosis.
- March 9, 2023: The FDA cleared the VITEK 2 AST-Gram Negative Fosfomycin (≤4 - ≥256 µg/mL) (K222430), a miniaturized, abbreviated and automated version of the classic broth dilution method to determine the minimum inhibitory concentration of Fosfomycin, an antibiotic used for the treatment of urinary tract infection.
- February 16, 2023: The FDA cleared the VITEK 2 AST-Gram Negative Plazomicin (≤0.5 – ≥16 μg/mL) (K223478), a miniaturized, abbreviated and automated version of the classic broth dilution method to determine the minimum inhibitory concentration of Plazomicin, an antibiotic used for the treatment of complicated urinary tract infection.
- February 9, 2023: The FDA cleared the VITEK 2 AST-Gram Negative Cefazolin (≤1 – ≥32 μg/mL) (K222073), a miniaturized, abbreviated and automated version of the classic broth dilution method to determine the minimum inhibitory concentration of Cefazolin, an antibiotic used for the treatment of various infections as well as for perioperative prophylaxis to reduce incidence of certain postoperative infections.
- February 3, 2023: The FDA cleared the VITEK 2 Streptococcus Tetracycline (≤ 0.25 - ≥ 16 μg/ml) (K223481), a miniaturized, abbreviated and automated version of the classic broth dilution method to determine the minimum inhibitory concentration of Tetracycline an antibiotic with updated breakpoints for testing Streptococcus pneumoniae, Streptococcus pyogenes (Group A Beta-Hemolytic streptococci) and Streptococcus spp. β-Hemolytic Group species.
- January 27, 2023: The FDA cleared the VITEK 2 AST-Gram Positive Moxifloxacin (≤0.25 - ≥ 8μg/ml) (K220803), a miniaturized, abbreviated and automated version of the classic broth dilution method to determine the minimum inhibitory concentration of Moxifloxacin an antibiotic with updated breakpoints for testing Enterococcus faecalis, Staphylococcus aureus and other Staphylococcus species.
- January 20, 2023: The FDA cleared the Sensititre YeastOne Susceptibility System with Caspofungin in the dilution range of 0.015-16ug/ml (K221899), a miniaturized version of the classic broth dilution method to determine the minimum inhibitory concentration of Caspofungin, an antifungal agent with updated breakpoints for testing Candida spp.
- January 18, 2023: The FDA cleared the Selux AST System; Model AST Gen 1.0 (K211759), a semi-automated and miniaturized version of the classic broth dilution method to simultaneously determine the minimum inhibitory concentration of 15 antimicrobials against select Enterococcus and Staphylococcus species, representing 35 different antimicrobial/organism combinations using the Selux Gram Positive Panel. Unlike traditional 96-well panels, the 384-well panel facilitates addition of new antimicrobials for testing as they become available.
- December 21, 2022: The FDA cleared the BD BBL Sensi-Disc Cefiderocol 30ug (FDC-30) (K221826), a disk diffusion assay for in vitro susceptibility testing of Cefiderocol, an antibiotic recently approved for the treatment of complicated urinary tract infections.
- October 13, 2022: The FDA cleared the VITEK 2 AST-Gram Positive Cefoxitin (K220805), a miniaturized, abbreviated and automated version of the doubling dilution technique designed to predict mecA-mediated oxacillin resistance in Staphylococcus spp.
- October 5, 2022: The FDA cleared an expanded indication for the Colibrí System (K220546), a semi-automated pre-analytical processor, to prepare microbial suspensions at a known concentration for antimicrobial susceptibility testing
- September 15, 2022: The FDA cleared the Thermo Scientific Oxoid Omadacycline Disc (30 ug) OMC30 (K203336), a disk diffusion assay for in vitro susceptibility testing of omadacycline, a new antibiotic for the treatment of community-acquired bacterial pneumonia (CABP) and acute bacterial skin and skin structure infections (ABSSSI).
- August 8, 2022: The FDA cleared the VITEK 2 AST- Gram Positive Telavancin (≤0.015 - ≥ µg/mL) (K212243), a miniaturized, abbreviated and automated version of the doubling dilution technique for determining the minimum inhibitory concentration of telavancin, an antibiotic used for the treatment of complicated skin and skin structure infections (cSSSI) and hospital-acquired and ventilator-associated bacterial pneumonia (HABP/VABP).
- July 12, 2022: The FDA cleared the VITEK 2 AST-Yeast Caspofungin (≤0.125 - ≥8 µg/mL) (K213899), a miniaturized, abbreviated and automated version of the classic broth dilution method to determine the minimum inhibitory concentration of caspofungin, an antifungal agent with updated breakpoints for testing Candida spp.
- June 3, 2022: The FDA cleared the VITEK 2 AST-Gram Negative Omadacycline (≤0.25 - ≥16 µg/mL) (K213931), a miniaturized, abbreviated and automated version of the classic broth dilution method to determine the minimum inhibitory concentration of omadacycline, a new antibiotic for the treatment of community-acquired bacterial pneumonia (CABP) and acute bacterial skin and skin structure infections (ABSSSI).
- April 29, 2022: The FDA granted the De Novo request for the BioFire Joint Infection (JI) Panel (DEN200066), a multiplexed nucleic-acid-based, in vitro diagnostic test intended for the simultaneous qualitative detection and identification of multiple bacterial and yeast nucleic acids and select antimicrobial resistance genes from synovial fluid obtained from individuals suspected to have a joint infection.
- April 27, 2022: The FDA cleared the EPlex Blood Culture Identification Gram Negative (BCID-GN) Panel (K213236), a multiplexed nucleic acid test intended for simultaneous qualitative detection and identification of multiple potentially pathogenic gram-negative bacterial organisms and select determinants associated with antimicrobial resistance, as well as detect several gram-positive bacteria and several Candida species all from positive blood culture. Claims were added to include the detection of nucleic acids from additional strains of E. coli, Citrobacter, Enterococcus, and Pseudomonas aeruginosa.
- April 14, 2022: The FDA cleared the VITEK 2 AST-Gram Negative Ciprofloxacin (≤0.06 - ≥4 µg/mL) (K214023), a miniaturized, abbreviated and automated version of the classic broth dilution method to determine the minimum inhibitory concentration of ciprofloxacin, an antibiotic with updated breakpoints for testing Enterobacterales and P. aeruginosa.
- February 25, 2022: The FDA cleared the VITEK 2 AST-Yeast Fluconazole (≤0.5 - ≥64 µg/mL) (K213241), a miniaturized, abbreviated and automated version of the classic broth dilution method to determine the minimum inhibitory concentration of fluconazole, an antifungal agent with updated breakpoints for testing Candida albicans, Candida parapsilosis, and Candida tropicalis.
- February 4, 2022: The FDA cleared the VITEK 2 AST-Gram Positive Linezolid (≤0.5 - ≥8 µg/mL) (K212849), a miniaturized, abbreviated and automated version of the classic broth dilution method to determine the minimum inhibitory concentration of linezolid, an antibiotic with updated breakpoints for testing Staphylococcus species
- December 20, 2021:The FDA cleared the Sensititre 18-24 Hour MIC or Breakpoint Susceptibility System with Cefiderocol in the Dilution Range of 0.03-64 µg/mL (K203741), a miniaturized version of the classic broth dilution method to determine the minimum inhibitory concentration of Cefiderocol with additional indicated species (Acinetobacter baumannii and Serratia marcescens) and using updated breakpoints for members of the Enterobacterales order.
- December 15, 2021:The FDA cleared the Sensititre YeastOne Susceptibility System with Voriconazole in the Dilution Range of 0.008 - 8 μg/mL (K211539), a micro-version of the broth dilution susceptibility test performed in multi-well microtiter plates to determine the minimum inhibitory concentration of voriconazole, an antifungal agent with new breakpoints and indications for testing Candida species.
- November 12, 2021: The FDA cleared the ETEST Fosfomycin (FO) (0.032-512 µg/mL) (K210757), a gradient diffusion assay to determine the minimum inhibitory concentration of Fosfomycin, an antibiotic used for the treatment of urinary tract infection.
- October 28, 2021: The FDA cleared the APAS Independence with IC Chromogenic MRSA BD Analysis Module and the APAS Independence with IC Chromogenic MRSA TFS/S Analysis Module (K200839), an in vitro diagnostic test system for the automated assessment of microbial colonies on chromogenic culture media to aid in screening for methicillin-resistant Staphylococcus aureus (MRSA).
- October 28, 2021: The FDA cleared the VITEK 2 AST- Streptococcus Cefotaxime (≤0.125 - ≥8 µg/mL) (K210287), an abbreviated and automated version of a broth microdilution assay to determine the minimum inhibitory concentration of Cefotaxime with Streptococcus species.
- October 27, 2021: The FDA cleared the Thermo Scientific Oxoid Lefamulin Disc (20µg) LMU20 (K210873), a disk diffusion assay for in vitro susceptibility testing of Lefamulin, a first-in-class antibiotic for the treatment of community-acquired bacterial pneumonia.
- October 20, 2021: The FDA cleared the MTS Piperacillin-Tazobactam 0.016/4 - 256/4 µg/mL (K211672), a gradient diffusion assay to determine the minimum inhibitory concentration of Piperacillin-Tazobactam, a combination antibiotic that is used to treat various bacterial infections.
- September 30, 2021: The FDA cleared the Acuitas AMR Gene Panel (K191288), a qualitative nucleic acid-based, highly multiplexed in vitro diagnostic test for the simultaneous detection and identification of 28 genetic determinants of resistance to 8 antibiotic groups (aminoglycosides, carbapenems, cephalosporins, fluoroquinolones, penicillins, sulfonamides, trimethoprim, vancomycin) among 19 organism species for a total of 117 unique organism/gene combinations being reported. The Acuitas AMR Gene Panel includes an extension of the device labeling (electronic user guide) that provides additional supporting information about performance characteristics and interpretation of genetic determinants associated with antimicrobial resistance for the Acuitas AMR Gene Panel.
- September 14, 2021: The FDA cleared the VITEK 2 AST-Gram Positive Fosfomycin (≤8 - ≥256 µg/mL) (K202396), an abbreviated and automated version of a broth microdilution assay to determine the minimum inhibitory concentration of Fosfomycin, an antibiotic used for the treatment of urinary tract infection.
- July 30, 2021: The FDA cleared the Thermo Scientific Oxoid Cefiderocol Disc (30ug) FDC30 (K203700), a disk diffusion assay for in vitro susceptibility testing of Cefiderocol, a newer antibiotic for the treatment of complicated urinary tract infection.
- July 23, 2021: The FDA cleared the Sensititre 20-24 hour Haemophilus influenzae /Streptococcus pneumoniae MIC or Breakpoint, Susceptibility System with Autoread Dtest (containing erythromycin at 1 ug/mL and clindamycin at 0.5 ug/mL) (K202612), a miniaturized version of the classic broth dilution method that can provide both qualitative and quantitative susceptibility results from Haemophilus influenza, Streptococcus pneumoniae and Streptococcus species when tested with erythromycin or clindamycin. The Dtest detects for inducible clindamycin resistance in Streptococcus spp. resistant to erythromycin.
- July 9, 2021: The FDA cleared the VITEK 2 AST-Gram Negative Meropenem (≤0.25 - ≥16 µg/mL) (K201675), an abbreviated and automated version of a broth microdilution assay to determine the minimum inhibitory concentration of Meropenem, an antibiotic for which FDA recently updated interpretive criteria.
- June 14, 2021: The FDA cleared the VITEK 2 AST-Gram Negative Imipenem/Relebactam (<0.25/4 - >16/4 µg/mL) (K211136), an abbreviated and automated version of a broth microdilution assay to determine the minimum inhibitory concentration of Imipenem/Relebactam. A claim was added to the previously cleared device to include a new indicated species, Acinetobacter calcoaceticus-baumannii complex.
- May 27, 2021: The FDA cleared the MicroScan MICroSTREP Plus Panels With Tetracycline (0.06-16 µg/mL) (K202423), an abbreviated version of a broth microdilution assay to determine the minimum inhibitory concentration of Tetracycline with aerobic streptococci. Performance data was updated to include reanalysis of MIC results for Streptococcus pneumoniae with tetracycline using currently recognized interpretive criteria.
- November 16, 2020: MicroScan Dried Gram-Negative MIC/Combo Panels with Ceftazidime (Caz) (0.5-64 μg/mL) (K202343), an abbreviated version of a broth microdilution assay to determine the minimum inhibitory concentration of Ceftazidime, a antibacterial used to treat lower respiratory tract infections, skin and skin-structure infections, bacterial septicemia, bone and joint infections, gynecologic infections, intra-abdominal infections and central nervous system infections
- September 28, 2020: VITEK 2 AST-Gram Negative Ceftazidime (≤0.5 - ≥32 µg/mL) (K193299) an abbreviated and automated version of a broth microdilution assay to determine the minimum inhibitory concentration of Ceftazidime, a antibacterial used to treat lower respiratory tract infections, skin and skin-structure infections, bacterial septicemia, bone and joint infections, gynecologic infections, intra-abdominal infections and central nervous system infections.
- September 15, 2020: Accelerate Pheno System, Accelerate PhenoTest BC Kit (K192665) a multiplexed in vitro diagnostic test utilizing both qualitative nucleic acid fluorescence in situ hybridization (FISH) identification and quantitative antimicrobial susceptibility methods directly from positive blood culture samples. Claims were added for antimicrobial susceptibility testing of Pseudomonas aeruginosa with ceftazidime, cefepime, meropenem, piperacillin/tazobactam, and aztreonam.
- June 29, 2020: Addition of Acinetobacter spp. for testing with the MicroScan Dried Gram-Negative MIC/Combo Panels with Meropenem (Mer) (0.004 - 32 µg/mL) (K201423), an abbreviated version of a broth microdilution assay to determine the minimum inhibitory concentration of Meropenem, an antibiotic for which FDA recently updated the susceptibility test interpretive criteria on the STIC website to include interpretive criteria when testing this organism group.
- May 7, 2020: ETEST Plazomicin (0.016 - 256 µg/mL) (K200512) a gradient diffusion assay to determine the minimum inhibitory concentration of Plazomicin, an antibiotic for the treatment of complicated urinary tract infection
- April 28, 2020: VITEK 2 AST-Gram Positive Delafloxacin (≤0.015 - ≥1 µg/mL) (K200590) an abbreviated and automated version of a broth microdilution assay to determine the minimum inhibitory concentration of Delafloxacin, an antibiotic approved for the treatment of community-acquired bacterial pneumonia (CABP) and acute bacterial skin and skin structure infections (ABSSSI)
- April 6, 2020: MTS Lefamulin 0.016 - 256 µg/mL (K200308) a gradient diffusion assay to determine the minimum inhibitory concentration of Lefamulin, a first-in-class antibiotic for the treatment of community-acquired bacterial pneumonia.
- March 20, 2020: MTS Omadacycline 0.002 - 32 µg/mL (K200180) a gradient diffusion assay to determine the minimum inhibitory concentration of Omadacycline, a new antibiotic for the treatment of community-acquired bacterial pneumonia (CABP) and acute bacterial skin and skin structure infections (ABSSSI).
- March 18, 2020: MicroScan Dried Gram Negative MIC/Combo Panels with Ciprofloxacin (Cp) (0.004 - 8 µg/mL) (K193536) an abbreviated version of a broth microdilution assay to determine the minimum inhibitory concentration of Ciprofloxacin, an antibiotic for which FDA recently recognized revised interpretive criteria and published those on the FDA STIC webpage.
- March 18, 2020: BioFire Blood Culture Identification 2 (BCID2) Panel (K193519) a multiplexed nucleic acid-based test for the detection and identification of multiple bacterial and yeast nucleic acids and select genetic determinants associated with antimicrobial resistance direct from positive blood culture samples.
- March 13, 2020: VITEK 2 AST-Gram Negative Imipenem/Relebactam (≤0.25/4 - ≥16/4 µg/mL) (K193572) abbreviated and automated version of a broth microdilution assay to determine the minimum inhibitory concentration of Imipenem/Relebactam, an antibiotic approved eight months ago for the treatment of complicated urinary tract infections and complicated intra-abdominal infections.
- March 12, 2020: Sensititre 18-24 hour MIC or Breakpoint Susceptibility System with Cefiderocol in the dilution range of 0.03-64 µg/mL (K193538) an abbreviated and automated version of a broth microdilution assay to determine the minimum inhibitory concentration Cefiderocol, an antibiotic approved four months ago for the treatment of complicated urinary tract infections.
- March 3, 2020: MicroScan Dried Gram-Negative MIC/Combo Panels with Levofloxacin (Lvx) (0.008 - 16 µg/mL) (K193358) an abbreviated version of a broth microdilution assay to determine the minimum inhibitory concentration of Levofloxacin, an antibiotic for which FDA recently recognized revised interpretive criteria and published those on the FDA STIC webpage.
- January 8, 2020: Sensititre 20-24 hour Haemophilus influenzae/Streptococcus Pneumoniae MIC or Breakpoint Susceptibility System with Lefamulin in the dilution range of 0.008 – 16 µg/mL (K193024) a broth-microdilution assay that was cleared shortly after new drug approval for Lefamulin, a first-in-class antibiotic for the treatment of community-acquired bacterial pneumonia.
- January 23, 2020: HardyDisk AST Cefiderocol 30µg (FDC30) (K193504) a disk diffusion assay that was the first AST device for Cefiderocol, an antibiotic for the treatment of complicated urinary tract infection. This device was cleared just eight weeks after new drug approval.
- December 20, 2019: The FDA recently cleared the Unyvero LRT BAL Application (K191967), a multiplex molecular test for the detection and identification of nucleic acid sequences from 20 bacterial/fungal pathogens and 10 antibiotic resistance markers to aid in the diagnosis of pneumonia. It is the first multiplexed pneumonia panel that identifies Pneumocystis jirovecii, a leading cause of pneumonia in immunocompromised patients.
- December 5, 2019: FDA authorizes marketing of diagnostic test that uses novel technology to detect MRSA bacteria - The FDA authorized marketing of a new diagnostic test based on bacterial viability and novel technology to detect Methicillin-resistant Staphylococcus aureus (MRSA) bacterial colonization, a widespread cause of hospital-acquired infections. The cobas vivoDx MRSA diagnostic test may allow health care professionals to evaluate patients for colonization with MRSA bacteria more quickly than traditional culture-based techniques when such testing is needed.
- November 26, 2019: The FDA cleared the AST device bioMerieux ETEST Delafloxacin (DFX) 0.002-32 μg/mL (K192738) a gradient diffusion assay for testing Delafloxacin
- November 14, 2019: The FDA cleared the AST device MicroScan Dried Gram Negative MIC/Combo Panels with Meropenem (Mer) (0.004-32 µg/mL) (K192355) a broth-microdilution assay for testing Meropenem.
- November 6, 2019: The FDA recently cleared AST devices for testing newly approved antimicrobial agents:
- HardyDisk AST Lefamulin 20µg (LMU20) (K192326) a disk diffusion assay for testing Lefamulin (September 19, 2019)
- ETEST Eravacycline (ERV) (0.002 – 32 Μg/ML) (K192050) a gradient diffusion assay for testing Eravacycline (September 29, 2019)
- Sensititre 18-24 Hour MIC Or Breakpoint Susceptibility System With Imipenem-Relebactam In The Dilution Range Of 0.03/4-256/4 Ug/ML (K192250) a broth-microdilution assay for testing Imipenem-Relebactam. (October 16, 2019) This device was evaluated under the auspices of the coordinated development guidance (issued on February 1, 2019) which aims at achieving timely availability of AST devices.
- AST device Sensititre 18-24 hour MIC or Breakpoint Susceptibility System with Lefamulin in the dilution range of 0.008 – 16 µg/mL (K192729) a broth-microdilution assay that was cleared just 80 days after new drug approval for Lefamulin, a first-in-class antibiotic for the treatment of community-acquired bacterial pneumonia. (November 6, 2019)
- October 31, 2019: The FDA cleared the AST device MTS Ampicillin-Sulbactam 0.016/0.008 – 256/128 µg/mL (K192345) a gradient diffusion assay for testing Ampicillin-Sulbactam.
- October 2, 2019: The FDA cleared NG Test CARBA 5 (K191889), the first rapid lateral flow immunochromatographic assay that detects and differentiates between five common types of carbapenemase enzymes (KPC, OXA, NDM, VIM, IMP). The assay tests pure colonies after growth on solid media, with results obtained in 15 minutes. The test is intended as an aid infection control.
- September 25, 2019: The FDA cleared ARIES MRSA assay (K191742), another nucleic acid amplification test (NAAT) for MRSA detection from nasal swabs. This and similar assays are used as an aid in the prevention and control of MRSA infections in healthcare settings.
Antimicrobial stewardship
The FDA works closely with domestic and international partners to promote the judicious use of antibiotics in the veterinary setting and complements the work done by other government agencies in the human healthcare setting.
On the veterinary side, the FDA’s Center for Veterinary Medicine (CVM) is responsible for:
- Ensuring that animal drugs are safe and effective for their approved conditions of use, and
- Playing an active role in coordinating the development and implementation of regulations and policies pertaining to antimicrobial drugs intended for use in animals, including food-producing animals.
CVM’s activities to advance antimicrobial stewardship are further detailed in CVM’s plan, Supporting Antimicrobial Stewardship in Veterinary Settings: Goals for Fiscal Years 2024-2028 (PDF, 2.5 MB). Also see: FDA Antimicrobial Stewardship in Animals: Stakeholder Resources and FDA-TRACK: Progress on FDA’s Support of Antimicrobial Stewardship in Veterinary Settings
On the human healthcare side, the FDA supports policies and regulations designed to preserve the effectiveness of antimicrobials for human use. This includes:
- Working to ensure the labeling of antimicrobial drugs intended for use in humans contain required statements regarding appropriate use
- Providing recommendations on scientifically sound clinical trial designs to evaluate human drugs to help inform appropriate use and stewardship efforts
- Maintaining the FDA-Recognized Antimicrobial Susceptibility Test Interpretive Criteria webpage
- Working with diagnostic manufacturers and academia on developing biomarkers to rapidly identify whether a patient’s symptoms are due to a bacterial infection, or when antibiotics can be stopped during treatment
- Promoting flexible regulatory approaches to rapid identification of bacterial pathogens, thereby allowing targeted antibiotic treatment and reducing broad-spectrum antibiotic use
Surveillance and monitoring of antimicrobial use and resistance
The FDA works in close coordination with interagency partners and domestic stakeholders to collect the data necessary to conduct surveillance and monitoring of antimicrobial use and resistance.
- A partnership between the FDA, the CDC, and the U.S. Department of Agriculture (USDA), the National Antimicrobial Resistance Monitoring System (NARMS) tracks and provides information on antimicrobial resistance in foodborne bacteria in humans, retail meats, and food-producing animals.
- NARMS Strategic Plan 2021-2025 (PDF, 127 KB) (August 19, 2020)
- NARMS Integrated Summary 2021
- The FDA is funding cooperative agreements to support collection of data on antimicrobial use in U.S. animal agriculture. The FDA has also provided input to USDA’s Center for Epidemiology and Animal Health on surveys to collect information on antimicrobial use in animal agriculture.
- Antimicrobial drug sponsors are required to report annually to the FDA the amounts of antimicrobial drugs sold or distributed for use in food-producing species during the prior year. The FDA’s Center for Veterinary Medicine publishes an annual report summarizing the data contained in those submissions.
- Most recent annual report: 2021 Summary Report on Antimicrobials Sold or Distributed for Use in Food-Producing Animals
- The FDA is leveraging in vitro diagnostic device data standards to enhance real-time infectious disease/AMR surveillance.
Regulatory science
The FDA supports regulatory science to develop the tools, standards, and approaches to facilitate the translation of breakthrough discoveries in science and technology into innovative, safe, and effective medical products.
The 2022: Advancing Regulatory Science at FDA: Focus Areas of Regulatory Science (FARS) report outlines topics FDA has identified as needing continued targeted investment in regulatory science research to facilitate development of innovative products, provide data and methods to inform regulatory decision-making, and improve guidance to sponsors. Antimicrobial resistance is a priority area, under the focus area “Public Health Preparedness and Response.” Please contact FARS@fda.hhs.gov with questions about this initiative.
- CDC-FDA Antimicrobial Resistance Isolate Bank (AR Isolate Bank)
- Database for Reference Grade Microbial Sequences (FDA-ARGOS)
- FDA Launches Resistome Tracker, an Interactive Research and Data Visualization Tool for Antibiotic Resistance Genes
- National Database of Antibiotic Resistant Organisms (NDARO), from NIH
- NARMS Now: Human Data
- GenomeTrakr Network
- NARMS Now Integrated Data
Community stakeholders: We need your samples
As part of our effort to address the global health challenge of AMR, the FDA supports the development of next-generation sequencing (NGS)-based diagnostics to help healthcare providers identify and treat the right pathogen. To help build NGS infrastructure, our FDA-ARGOS database makes publicly available quality-controlled microbial reference genomes for diagnostic use. The FDA team is looking for unique, hard-to-source microbes like biothreat organisms, emerging pathogens, and AMR-related pathogens to help improve the database. We encourage the community to share microbe samples.
The Center for Drug Evaluation and Research
- CDER's Office of Antimicrobial Products research activities include facilitating the development of new antibacterial drugs to treat patients and advancing the science of clinical trial design.
- Exploiting Real-World Data to Optimize the Use of Antibiotics - Through the National Action Plan for Combating Antibiotic-Resistant Bacteria (CARB) (PDF, 370KB - research summary published Nov. 2021), FDA's Center for Drug Evaluation and Research (CDER) has supported research at Johns Hopkins University School of Medicine to help us use the data in electronic health records to better understand the association between varying durations of antibiotic therapy and patient outcomes. These two research studies demonstrated the feasibility and advantages of a novel automated approach for extracting patient-level data from electronic health records to capture treatment outcomes in diverse real-world health care settings. The results provide valuable evidence to inform best practices related to the duration of antibiotic treatment in diverse bacterial infections, optimizing patient outcomes while reducing the risk for antimicrobial resistance.
The Center for Biologics and Evaluation and Research
- Research enabling development of new vaccines against tuberculosis:
- Research to facilitate development of vaccines against Staphylococcus aureus (e.g. MRSA):
The National Center for Toxicological Research’s Division of Microbiology
Center for Veterinary Medicine
- April 26, 2024: The FDA’s Center for Veterinary Medicine finalized Guidance for Industry (GFI) #120: Veterinary Feed Directive Regulation Questions and Answers, to assist stakeholders involved with veterinary feed directives (VFDs) – veterinarians, VFD feed distributors (medicated feed mills, feed retailers) and clients (owners or other caretakers of the animals) – in complying with the Veterinary Feed Directive (VFD) final rule that published in 2015. The VFD final rule outlines the process for authorizing the use of approved animal drugs in the feed of food-producing animals that require veterinary oversight, including medically important antimicrobials when needed for specific animal health purposes. This final guidance also serves as a Small Entity Compliance Guide.
- March 5, 2024: The FDA is accepting proposals through May 13, 2024 for cooperative agreement funding to support the collection of antimicrobial use data from diverse animal sectors. The cooperative agreements provide up to three awards in fiscal year (FY) 2024 for a total of $600,000, and up to five awards in FY 2025 for a total of $1,000,000. The funding opportunities are the FDA’s latest step toward collecting information about the use of antimicrobials in animals.
- Regulatory Science Extramural Research and Development Projects
- CARB-X - CARB-X is a non-profit public-private partnership dedicated to accelerating antibacterial research to tackle the global rising threat of drug-resistant bacteria. CARB-X welcomes applications from around the world for funding and support for the early development of antibiotics, diagnostics, vaccines, devices, and other products to combat the most serious drug-resistant bacteria. Visit the CARB-X website for information on application deadlines.
FDA publications
Guidance documents, compliance policy guides, and other FDA publications represent the FDA's current thinking on a topic. Documents related to antimicrobial resistance in humans and animals include guidances on developing products for treatment, prevention, and diagnosis of bacterial infections. You can also find information for the animal and veterinary industry on collection of sales and distribution of antimicrobial products, and veterinary feed directives.
You can search the entire database of FDA guidance documents by keyword, or visit the industry pages below for more information.
For information about FDA-recognized antimicrobial susceptibility test interpretive criteria, visit http://www.fda.gov/STIC, and the corresponding Notice of Updates.
- November 29, 2022: The FDA announced the availability of a final guidance entitled Enforcement Policy Regarding Investigational New Drug Requirements for Use of Fecal Microbiota for Transplantation to Treat Clostridioides difficile Infection Not Responsive to Standard Therapies; Guidance for Industry. The guidance document informs members of the medical and scientific community and other interested persons notice that, at this time, FDA intends to exercise enforcement discretion with respect to the investigational new drug application (IND) requirements for the use of fecal microbiota for transplantation (FMT) to treat Clostridioides difficile (C. difficile) infection not responding to standard therapies under limited circumstances described in the guidance.
- October 28, 2022: The FDA published a draft guidance for industry entitled Clostridioides difficile Infection: Developing Drugs for Treatment, Reduction of Recurrence, and Prevention. The purpose of this draft guidance is to assist sponsors in the clinical development of drugs for the treatment of Clostridioides difficile infection (CDI), reduction of recurrence, or prevention of CDI.
- September 12, 2022: Monkeypox response: The FDA released additional information in publicly posted reviews supporting approval of the new drug application for tecovirimat to describe specific changes in the VP37 proteins of orthopoxviruses (e.g., vaccinia virus and monkeypox virus) that are associated with tecovirimat drug resistance. FDA is releasing this information to aid the scientific community’s genomic sequencing efforts to support national surveillance of the current monkeypox virus outbreak in the U.S. We believe this additional information will further facilitate the ability to monitor for the development and spread of tecovirimat-resistant virus and therefore is important in promoting public health. Additional information on FDA’s response to the public health emergency, including summary information on tecovirimat drug resistance, is available at: FDA Monkeypox Response.
- May 24, 2022: The FDA announced the availability of a draft guidance for industry entitled Antibacterial Therapies for Patients With an Unmet Medical Need for the Treatment of Serious Bacterial Diseases--Questions and Answers (Revision 1). The purpose of this draft guidance is to assist sponsors in the clinical development of new antibacterial drugs, and it provides updates to the options for development programs, given the availability of some new therapeutic options. This draft guidance will provide necessary updates to the final guidance entitled Antibacterial Therapies for Patients With an Unmet Medical Need for the Treatment of Serious Bacterial Diseases published on August 2, 2017.
- November 9, 2021: Exploiting Real-World Data to Optimize the Use of Antibiotics
- October 2021: FDA CDER Office of Infectious Diseases CARB Research Overview Fiscal Years 2016-2021 (PDF, 370 KB)
- August 28, 2020: The FDA updated omadacycline disk breakpoints for Streptococcus pneumoniae for community acquired bacterial pneumonia and updated susceptibility test interpretive criteria for daptomycin (rationale).
- August 5, 2020: The FDA issued a final guidance, Limited Population Pathway for Antibacterial and Antifungal Drugs.
- June 29, 2020: The FDA issued a draft guidance, Development of Anti-Infective Drug Products for the Pediatric Population.
- June 24, 2020: The FDA issued two final guidances, Hospital-Acquired Bacterial Pneumonia and Ventilator-Associated Bacterial Pneumonia: Developing Drugs for Treatment, and Community-Acquired Bacterial Pneumonia: Developing Drugs for Treatment.
- December 23, 2019: The FDA has recognized the standard for Acinetobacter spp. for meropenem.
- September 5, 2019: The FDA has added pretomanid and lefamulin to the antibacterial susceptibility test interpretive criteria web page. The FDA identified susceptibility test interpretive criteria for lefamulin, which can be found on the antibacterial susceptibility test interpretive criteria web page. There are no identified susceptibility test interpretive criteria for pretomanid at this time.
- July 26, 2019:The FDA has added imipenem-cilastatin-relebactam to the antibacterial susceptibility test interpretive criteria web page.
- July 18, 2019: The FDA finalized a guidance document, Submitting Next Generation Sequencing Data to the Division of Antiviral Products Guidance for Industry Technical Specifications Document. The purpose of this technical specifications document is to provide the current thinking of FDA’s Division of Antiviral Products in regard to the submission of next generation nucleotide sequence analysis procedures and data in support of resistance assessments for the development of antiviral drug products. Providing accurate resistance information is imperative for protecting public health to prevent the emergence of novel resistant and cross-resistant viral variants that have the potential to infect others and cause major outbreaks of disease that cannot be controlled by approved drug products.
- February 2, 2018: Report to Congress on Generating Antibiotic Incentives Now (GAIN) (PDF, 545KB)
- In November 2023, the FDA issued a proposed rule to classify certain wound dressings and wound washes that contain antimicrobials and other chemicals, based on the level of antimicrobial resistance concern. The proposed classification for these wound dressings and liquid wound washes is intended to be split into two classifications: while most of these products are proposed to be classified into class II (subject to special controls, in combination with general controls, and requiring a premarket notification), those products that contain a medically important antimicrobial are proposed to be classified into class III (requiring a PMA to provide a reasonable assurance of safety and effectiveness, as detailed in the accompanying proposed order).
- In September 2023, the FDA issued “Antimicrobial Susceptibility Test (AST) System Devices–Updating Breakpoints in Device Labeling” as an immediately-in-effect guidance. This guidance is intended to provide industry and FDA staff with information regarding updating susceptibility test interpretive criteria (STIC)/breakpoints and associated performance data in device labeling for antimicrobial susceptibility test (AST) system devices.
- In May 2023, the FDA launched a new web page, Antimicrobial Resistance and Medical Devices, to explain how antimicrobial susceptibility test devices are intended to help health care providers identify the correct therapy (antimicrobial agent) to treat specific bacterial or fungal infections and help identify drug-resistant infections for patient care. Antimicrobial susceptibility testing devices sold in the U.S. for use in clinical laboratories must be reviewed and cleared by the FDA’s Center for Devices and Radiological Health (CDRH).
- 510(k) Premarket Notification and de novo databases – provide information on all in vitro diagnostic devices cleared or granted since November 2003, including devices that detect antibiotic resistance markers, phenotypic antimicrobial susceptibility devices, and biomarkers used to aid in patient management
- Part of the FDA's strategic approach for combatting antimicrobial resistance involves providing guidance that aims to facilitate the availability of antimicrobial susceptibility tests in a timely manner once a new antibacterial drug is approved. On January 17, 2019, the FDA published a new guidance for industry, Coordinated Development of Antimicrobial Drugs and Antimicrobial Susceptibility Test Devices. The goal of this guidance is to minimize time between the approval of new antimicrobial drugs and clearance of antimicrobial susceptibility tests used to determine the potential effectiveness of those drugs; and provide recommendations to the medical device and drug industries on how to work together to facilitate timely clearance of antimicrobial susceptibility test devices by the FDA. (Federal Register notice)
- October 10, 2024: The FDA announced the publication of the 2023 Summary Report on Antimicrobials Sold or Distributed for Use in Food-Producing Animals. The 2023 data indicate that U.S. sales and distribution of medically important antimicrobial drugs approved for use in food-producing animals decreased by 2% between 2022 and 2023; this represents a 37% decrease in sales since the sales peaked in 2015.
- December 7, 2023: The FDA's Center for Veterinary Medicine released the 2022 Summary Report on Antimicrobials Sold or Distributed for Use in Food-Producing Animals. This year’s data show that domestic sales and distribution of medically important antimicrobial drugs approved for use in food-producing animals increased by four percent between 2021 and 2022; compared to 2015 (peak year of sales), 2022 sales were down 36 percent. The agency also updated the Interactive Summary of Biomass-Adjusted Antimicrobial Sales Data to include 2022 data.
- November 22, 2023: In response to requests filed by stakeholders, the FDA is extending the comment period for Draft GFI #273, “Defining Durations of Use for Approved Medically Important Antimicrobial Drugs Fed to Food-Producing Animals,” for an additional 10 days. The comment period will now close on January 5, 2023. For additional information, see: Defining Durations of Use for Approved Medically Important Antimicrobial Drugs Fed to Food-Producing Animals; Draft Guidance for Industry; Availability; Extension of Comment Period.
- November 20, 2023: The FDA Center for Veterinary Medicine published a Perspectives with CVM blog post, CVM Antimicrobial Stewardship in FY 2023 and Beyond, in recognition of 2023 World Antimicrobial Awareness Week (November 18-24). The post highlights what CVM is doing to address antimicrobial resistance and preserve the effectiveness of these critical and life-saving drugs.
- September 27, 2023: FDA Releases Plan for Supporting Antimicrobial Stewardship in Veterinary Settings for FY 2024-2028. The FY 2024-2028 plan is a continuation of the previous 5-plan (implemented through 2019-2023) and aims to limit or reverse resistance arising from the use of antibiotics in animals, while continuing to ensure the availability of safe and effective antibiotics for use in animals and humans.
- March 6, 2023: In December 2022, the FDA’s Center for Veterinary Medicine released a draft update to guidance for industry (GFI) #152, “Evaluating the Safety of Antimicrobial New Animal Drugs with Regard to Their Microbiological Effects on Bacteria of Human Health Concern.” The guidance is a tool for assessing the risk of AMR in people, which could result from the use of a medically important antimicrobial drug in food-producing animals. The scope and purpose of updated GFI #152 remains the same as the initial version of the guidance issued in 2003, but updates better align with current science and clinical practices in human medicine.
- December 16, 2022: The FDA’s Center for Veterinary Medicine released a draft update to guidance for industry (GFI) #152, “Evaluating the Safety of Antimicrobial New Animal Drugs with Regard to Their Microbiological Effects on Bacteria of Human Health Concern.” The guidance is a tool for assessing the risk of antimicrobial resistance (AMR) in people, which could result from the use of a medically important antimicrobial drug in food-producing animals. The scope and purpose of updated GFI #152 remains the same as the initial version of the guidance issued in 2003, but updates better align with current science and clinical practices in human medicine.
- December 12, 2022: The FDA's Center for Veterinary Medicine published the 2021 Summary Report on Antimicrobials Sold or Distributed for Use in Food-Producing Animals. This year’s report shows that domestic sales and distribution of medically important antimicrobial drugs approved for use in food-producing animals decreased by less than one percent between 2020 and 2021.
- November 29, 2022: The FDA’s Center for Veterinary Medicine launched an Interactive Summary of Biomass-Adjusted Antimicrobial Sales Data. The display applies a biomass denominator to adjust existing annual antimicrobial sales and distribution data for medically important antimicrobial drugs sold or distributed for use in food-producing animals in the U.S. for years 2016 to 2020. Animal biomass is defined as the population of a given livestock species in the U.S. multiplied by the average weight of that species. In this method, a biomass denominator adjusts annual antimicrobial sales data to account for the size of the population of a given livestock species in the U.S. potentially being treated with those drugs.
- June 30, 2022: The FDA’s Center for Veterinary Medicine released both a status update (PDF, 273 KB) on Phase I of its five-year action plan for Supporting Antimicrobial Stewardship in Veterinary Settings as well as a report (PDF, 12.8 MB) to describe some of the data that FDA and federal partners collect regarding antimicrobial sales, use, and resistance in U.S. animal agriculture and the related food chain.
- FDA issues draft guidance to voluntarily bring remaining approved over-the-counter medically important antimicrobial drugs for animals under veterinary oversight (September 23, 2019) - The FDA released the draft guidance for industry #263 Recommendations for Sponsors of Medically Important Antimicrobial Drugs Approved for Use in Animals to Voluntarily Bring Under Veterinary Oversight All Products That Continue to be Available Over-the-Counter, to help explain the recommended process for voluntarily bringing the limited number of remaining approved animal drugs containing antimicrobials of human medical importance (i.e., medically important) under the oversight of licensed veterinarians by changing the approved marketing status from over-the-counter to prescription.
- FDA-TRACK: Progress on FDA’s Support of Antimicrobial Stewardship in Veterinary Settings
- Antimicrobial Resistance Guidances – information for animal and veterinary industry
- Veterinary Feed Directive
- FDA’s Proposed Method for Adjusting Data on Antimicrobials Sold or Distributed for Use in Food-Producing Animals Using a Biomass Denominator (PDF, 174 KB)
Information for consumers
- Animation of Antimicrobial Resistance (video, 9 minutes – text version also available)
- Antimicrobial Resistance in animals
- Questions and Answers: Summary Report on Antimicrobials Sold or Distributed for Use in Food-Producing Animals
- Antibiotic/Antimicrobial Resistance - information from the CDC
- Presidential Advisory Council on Combating Antibiotic-Resistant Bacteria (PACCARB) - provides advice, information, and recommendations to the HHS Secretary regarding programs and policies intended to support and evaluate the implementation of U.S. government activities related to combating antibiotic-resistant bacteria
Press and statements
- January 8, 2025: The FDA released a request for comments (RFC) soliciting public input on new opportunities and emergent monitoring needs for possible inclusion in the forthcoming National Antimicrobial Resistance Monitoring System (NARMS) 2026-2030 Strategic Plan. The Federal Register notice about the RFC includes instructions for submitting comments, as well as specific questions and requests for information meant to prompt helpful submissions. The 75-day comment period will be open from January 10 to March 26, 2025.
- October 10, 2024: The FDA announced the publication of the 2023 Summary Report on Antimicrobials Sold or Distributed for Use in Food-Producing Animals. The 2023 data indicate that U.S. sales and distribution of medically important antimicrobial drugs approved for use in food-producing animals decreased by 2% between 2022 and 2023; this represents a 37% decrease in sales since the sales peaked in 2015.
- September 25, 2024: The FDA announced it is awarding funds for three projects to collect, analyze and report data on antimicrobial use (AMU) in animals. These projects support long term AMU data collection efforts under development within the U.S, including proposed public-private partnership frameworks for tracking AMU data.
- July 15, 2024: The FDA authorized marketing of DiaSorin Molecular LLC’s Simplexa C. auris Direct, a molecular-based assay intended to detect Candida auris (C. auris) DNA from a skin swab of the armpit or groin from patients suspected of C. auris colonization. The test is intended to help prevent and control C. auris infections in health care settings. The assay may allow health care professionals to evaluate patients for colonization with C. auris faster than traditional culture-based techniques when such testing is needed. Faster detection can help stop the spread of this organism, which is frequently resistant to multiple antifungal drugs and can cause serious infections in hospitalized patients. Test results are meant to be used in conjunction with other clinical, epidemiologic, and laboratory information available to the clinician evaluating the patient. The test is not intended to diagnose or monitor treatment for C. auris infection. This is the latest example of the FDA’s ongoing commitment to helping ensure the development and expansion of tests for emerging infectious pathogens.
- June 21, 2024: The FDA converted Sirturo (bedaquiline) to traditional approval following a determination that a confirmatory trial verified clinical benefit. Sirturo is indicated for pulmonary tuberculosis (TB) due to Mycobacterium tuberculosis resistant to at least rifampin and isoniazid, also known as multi-drug resistant tuberculosis (MDR-TB), as part of a combination therapy, for adults and pediatric patients (5 years and older, weighing at least 15 kg). Sirturo was first approved in December 2012 under the FDA’s Accelerated Approval pathway. As part of the initial approval, the FDA required the applicant to conduct a confirmatory clinical study and develop a patient registry to assess rates of serious adverse events.
- April 24, 2024: FDA Approves New Treatment for Uncomplicated Urinary Tract Infections - The FDA approved Pivya (pivmecillinam) tablets for the treatment of female adults with uncomplicated urinary tract infections (UTIs) caused by susceptible isolates of Escherichia coli, Proteus mirabilis and Staphylococcus saprophyticus.
- April 9, 2024: FDA Approves New Antimicrobial Drug for Cattle and Swine - The FDA approved Pradalex (pradofloxacin injection) solution for certain respiratory diseases in cattle and swine. Pradofloxacin is a medically important antimicrobial in the fluoroquinolone class and may only be prescribed by a licensed veterinarian as a single injection. Over the past several decades, FDA has implemented policies to help ensure that medically important antimicrobials approved for use in animals are used in a manner that is consistent with principles of antimicrobial stewardship. For example, all medically important antimicrobials for animals require the authorization of a licensed veterinarian because FDA believes that, given their specialized training and experience, veterinarians play a critical role in antimicrobial stewardship and can help reduce the risks of antimicrobial resistance.
- April 3, 2024: The FDA approved Zevtera (ceftobiprole medocaril sodium for injection) for the treatment of adults with Staphylococcus aureus bloodstream infections (bacteremia) (SAB), including those with right-sided infective endocarditis; adults with acute bacterial skin and skin structure infections (ABSSSI); and adult and pediatric patients three months to less than 18 years old with community-acquired bacterial pneumonia (CABP). For more information, see the FDA press release: FDA Approves New Antibiotic for Three Different Uses.
Events
Recent and upcoming AMR-related events involving the FDA will be listed here.
- April 17, 2023: Antimicrobial Drugs Advisory Committee meeting (virtual) - The committee met in open session to discuss new drug application (NDA) 216974, for sulbactam-durlobactam for injection, submitted by Entasis Therapeutics, Inc. The applicant's proposed indication was for the treatment of infections due to Acinetobacter baumannii-calcoaceticus complex including multidrug-resistant and carbapenem-resistant strains.
- February 9, 2023: FDA Grand Rounds: A Modular Approach for Enhanced Plasmid Subtyping and AMR Gene Profiling of Plasmids (webcast, 12:00 - 1:00 p.m. ET) - Plasmids are a major factor in the spread of antimicrobial resistance genes. Current plasmid typing methods do not account for the great degree of genetic diversity associated with the recombination mechanisms that allow plasmids to acquire antimicrobial resistance genes. In this presentation by Lucas Harrison, Ph.D., FDA Center for Veterinary Medicine (CVM), we introduce an enhanced plasmid subtyping method that not only identifies the genetic elements exclusive to and indicative of a plasmid type, but also characterizes plasmids based on the DNA sequence and relative position of these genetic elements as they are rearranged through plasmid recombination mechanisms.
- November 8, 2022: Maximizing Benefits and Minimizing Harms from Antibiotics: Scientific, Regulatory and Clinical Considerations by Dr. Sara Cosgrove (webcast, 3:00 - 4:00 p.m. ET), hosted by the Johns Hopkins University Center of Excellence in Regulatory Science and Innovation (CERSI). This presentation will address approaches to optimize antibiotic use through antibiotic stewardship including updates regarding federal regulations, strategies to enhance antibiotic stewardship and minimize antibiotic-associated adverse events throughout all healthcare settings, and approaches to change attitudes and behavior around antibiotic prescribing.
- September 22, 2022: Vaccines and Related Biological Products Advisory Committee meeting (virtual, 8:30 a.m. - 5:00 p.m. ET) - The committee will meet in open session to discuss the Biologics License Application # 125739 (BLA - 125739) from Rebiotix Inc. for a product, Rebyota (Fecal Microbiota, Live), with a requested indication to reduce the recurrence of Clostridioides difficile infection (CDI) in adults following antibiotic treatment for recurrent CDI.
- September 20-22, 2022: 2022 Public Meeting of the National Antimicrobial Resistance Monitoring System (NARMS) - The NARMS public meeting will be held virtually on Wednesday, September 21, 2022 from 12:00 p.m. to 5:00 p.m. ET and Thursday, September 22, 2022 from 9:30 a.m. to 4:30 p.m. ET. A virtual technical workshop to demonstrate how to access NARMS data online will be held on Tuesday September 20, 2022 from 9:00 a.m. to 4:00 p.m. ET. For more information, also see: FDA Announces 2022 Public Meeting of the National Antimicrobial Resistance Monitoring System.
- August 30, 2022: Virtual public workshop - Drug Development Considerations for the Prevention of Healthcare-Associated Infections - FDA and the Centers for Disease Control and Prevention (CDC) are co-sponsoring this workshop to discuss topics including the current state of development of pathogen-directed products used to prevent healthcare-associated infections, and antimicrobial resistance threats as potential targets for decolonization and pathogen reduction.
- June 22-23, 2022: The National Institute of Allergy and Infectious Diseases (NIAID) will host a virtual workshop: Strategies for Early-Stage Programs Developing Novel Antibacterial and Antifungal Drugs, including some FDA speakers. This workshop is intended primarily for academic groups or small start-ups with limited practical experience in all stages of therapeutics product development. The focus will be on the early phases of product development for antibacterial and antifungal agents, starting after discovery phase when leads have been identified. Workshop attendees should be in the early stages of product development and should have an identified product, library, or scaffold that they are interested in developing into a therapeutic treatment or should be supporting early product development activities through their organization.
- June 14, 2022: Exploring the Potential for a Public-Private Partnership to Support the Tracking and Monitoring of Antimicrobial Use in Food-Producing Animals, virtual public forum, 1:00 - 3:00 p.m. ET, hosted by the Reagan-Udall Foundation for the Food and Drug Administration. Please register in advance.
- June 3, 2022: Development Considerations of Antimicrobial Drugs for the Treatment of Uncomplicated Urinary Tract Infections (UTI) (virtual) - The workshop will focus on nonclinical and clinical considerations regarding antimicrobial drug development for uncomplicated UTI.
- October 7, 2021: The Antimicrobial Drugs Advisory Committee will meet via webcast. The committee will discuss new drug application (NDA) 215596, for maribavir oral tablets, submitted by Takeda Pharmaceuticals USA, Inc., for the treatment of adults with post-transplant cytomegalovirus infection and/or disease, including infections resistant and/or refractory to ganciclovir, valganciclovir, cidofovir, or foscarnet. (Federal Register notice)
- August 30 - September 1, 2021: Science and Regulation of Bacteriophage Therapy workshop (virtual) - FDA's Center for Biologics Evaluation and Research, and the National Institutes of Health, National Institute of Allergy and Infectious Diseases (NIH/NIAID) are hosting a public workshop to exchange information with the medical and scientific community about the regulatory and scientific issues associated with bacteriophage therapy.
- April 23, 2021: Development Considerations of Antimicrobial Drugs for the Treatment of Gonorrhea (virtual workshop), hosted by FDA, NIAID, and CDC to discuss the nonclinical and clinical pharmacology data and clinical trial design considerations regarding developing antimicrobial drugs for the treatment of gonorrhea.
Interagency collaboration to address AMR
FDA participates in and contributes to Combating Antibiotic-Resistant Bacteria (CARB), a Government-wide effort launched in 2014, including the work of:
- On October 9, 2020, the Interagency Task Force for CARB released the National Action Plan for Combating Antibiotic-Resistant Bacteria, 2020-2025, which presents coordinated, strategic actions that the United States Government will take in the next five years to improve the health and wellbeing of all Americans by changing the course of antibiotic resistance. This plan is based on the U.S. Government’s 2014 National Strategy for CARB, and builds on the first National Action Plan released in 2015 by expanding evidence-based activities that have already been shown to reduce antibiotic resistance, such as optimizing the use of antibiotics in human and animal health settings.
- The Presidential Advisory Council on Combating Antibiotic-Resistant Bacteria (PACCARB) that provides advice, information, and recommendations to the Department of Health and Human Services (HHS) Secretary related to combating AMR.
The FDA’s Office of Public Health Strategy and Analysis (OPHSA) coordinates the FDA’s involvement in CARB and represents the FDA on PACCARB. Based on consultation with and input from the FDA’s Centers, OPHSA routinely updates HHS on the FDA’s progress in meeting National Action Plan goals, objectives, and milestones.
Contact the FDA
Consumers and general information: contact FDA
You may also call 1-888-INFO-FDA / (1-888-463-6332)
Report a fraudulent product
Includes options for phone and online reporting
Press: contact the Office of Media Affairs
Email fdaoma@fda.hhs.gov or call 301-796-4540

