Drug Trials Snapshot: POSLUMA
HOW TO USE THIS SNAPSHOT
The information provided in Snapshots highlights who participated in the key clinical trials that supported the original FDA approval of this drug, and whether there were differences among sex, race, age, and ethnic groups. The “MORE INFO” bar shows more detailed, technical content for each section. The Snapshot is intended as one tool for consumers to use when discussing the risks and benefits of the drugs.
LIMITATIONS OF THIS SNAPSHOT
Do not rely on Snapshots to make decisions regarding medical care. Always speak to your healthcare provider about the benefits and risks of a drug.
Some of the information in this Snapshot is for presentation purposes and does not represent the approved conditions of use of this drug. Refer to the POSLUMA Prescribing Information for all of the approved conditions of use of this drug (e.g., indication(s), population(s), dosing regimen(s), safety information).
Snapshots are limited to the information available at the time of the original approval of the drug and do not provide information on who participated in clinical trials that supported later approvals for additional uses of the drug (if applicable).
POSLUMA (flotufolastat F 18)
(Pos-lum-ah)
Blue Earth Diagnostics
Approval date: May 25, 2023
DRUG TRIALS SNAPSHOT SUMMARY:
What is the drug for?
POSLUMA is a drug used for detecting specific cancer lesions in males with prostate cancer, specifically:
- whose newly diagnosed cancer could be cured with the initial treatment, or
- who have been treated for prostate cancer but have high prostate-specific antigen (PSA) in their blood. High PSA in the blood of these patients is a suspicious sign that cancer is coming back or spreading.
How is this drug used?
POSLUMA is an injection given by a health care provider in the vein (intravenous) in preparation for an imaging test that can help detect cancer (called positron emission tomography or PET scan imaging).
Who participated in the clinical trials?
The FDA approved POSLUMA based on evidence from two clinical trials (Trial 1/NCT04186819 and Trial 2/NCT04186845) of 747 male patients with prostate cancer. Trial 1 included 356 patients with newly diagnosed prostate cancer. Trial 2 included 391 patients who were treated for prostate cancer before, but there was suspicion that the cancer was spreading because of rising PSA.
Trial 1 was conducted at 34 sites in the United States, Finland, Germany, and the Netherlands. Trial 2 was conducted at 28 sites in the United States, Finland, and the Netherlands.
How were the trials designed?
There were two trials that evaluated benefits and side effects of POSLUMA.
Trial 1 enrolled patients who were recently diagnosed with unfavorable intermediate-risk, high-risk, or very high-risk prostate cancer and were awaiting surgery for the removal of the prostate and the nearby lymph nodes.
Trial 2 enrolled patients who were already treated for prostate cancer but had rising PSA levels, suspicious for cancer recurrence.
The benefit of POSLUMA in Trial 1 was evaluated by measuring the successful detection of cancer lesions in the pelvis using POSLUMA PET or computed tomography (CT) imaging in comparison to post-surgery lymph tissue results (histopathology of the pelvic lymph nodes).
The benefit of POSLUMA in Trial 2 was evaluated by comparing the agreement in cancer lesion detection between images done with POSLUMA PET/CT imaging and one of the standard tests (imaging or tissue biopsy) for detecting cancer recurrence.
How were the trials designed?
The safety and efficacy of POSLUMA were evaluated in two prospective, open-label trials (Trial 1 and Trial 2) in males with prostate cancer.
Trial 1 enrolled patients with biopsy-proven prostate cancer who were scheduled for radical prostatectomy and pelvic lymph node dissection. Patients underwent POSLUMA PET/CT imaging followed by surgery. The images were interpreted by three blinded independent readers and compared to histopathology obtained following surgical removal of pelvic lymph nodes.
Trial 2 enrolled patients with biochemical evidence of recurrent prostate cancer after definitive therapy defined by two serum PSA measurements of >0.2 ng/mL more than six weeks after prostatectomy or by an increase in serum PSA of at least 2 ng/mL above nadir after definitive radiotherapy. All patients received a single POSLUMA PET/CT imaging. The images were interpreted by three blinded independent readers and compared to at least one of the following: histopathology or imaging (CT, magnetic resonance imaging [MRI], bone scan, or fluciclovine F 18 PET) obtained within 90 days of the POSLUMA scan.
DEMOGRAPHICS SNAPSHOT:
Figure 1. Baseline Demographics by Sex
Source: Adapted from FDA Review
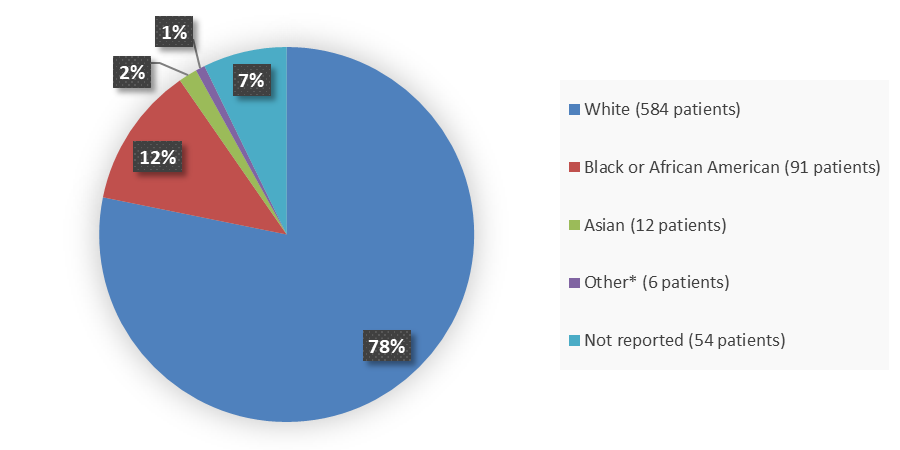
Figure 2. Baseline Demographics by Race
Source: Adapted from FDA Review
*Other includes American Indian or Alaska Native (3 patients), Native Hawaiian or other Pacific Islander (2 patients), and other (1 patient).
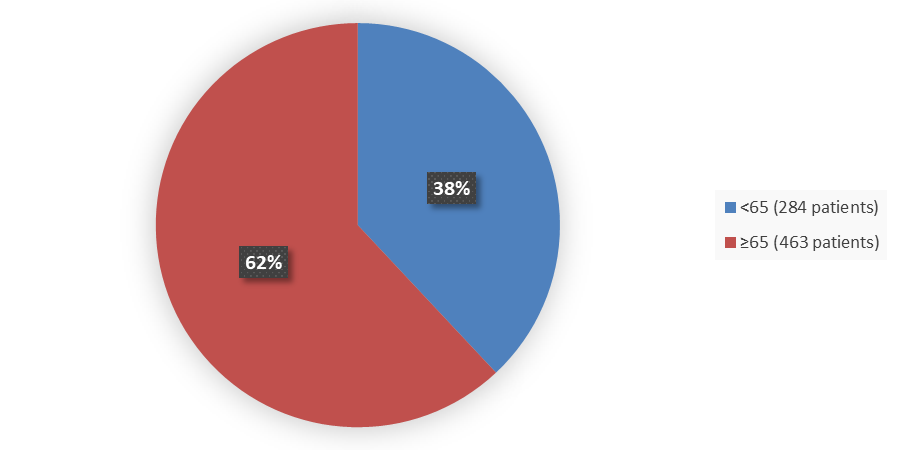
Figure 3. Baseline Demographics by Age
Source: Adapted from FDA Review
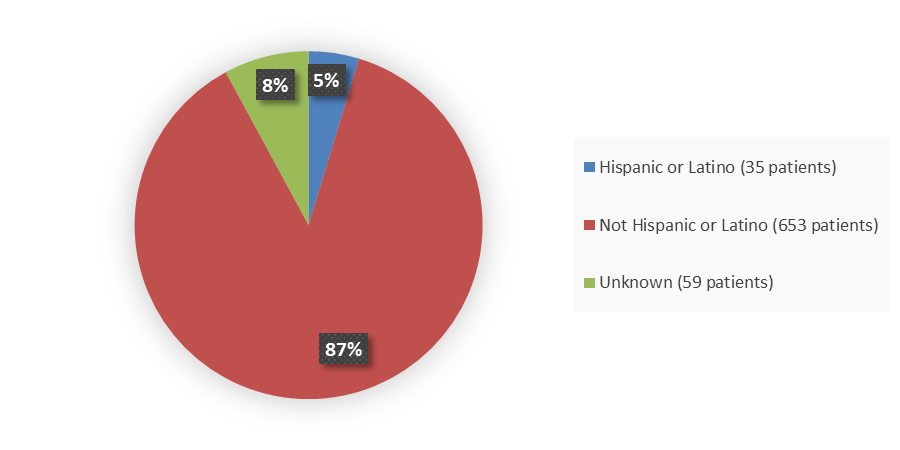
Figure 4. Baseline Demographics by Ethnicity
Source: Adapted from FDA Review
Who participated in the trials?
Table 1 summarizes demographics of patients in the clinical trials of POSLUMA.
Table 1. Demographics of Patients in the Clinical Trials
|
Demographic Parameters |
Trial 1 N=356 |
Trial 2 N=391 |
Total N=747 |
|---|---|---|---|
|
Sex, n (%) |
|
|
|
|
Male |
356 (100) |
391 (100) |
747 (100) |
|
Age, years |
|
|
|
|
Median |
65.0 |
69.0 |
67.0 |
|
Min, max |
46, 83 |
43, 86 |
43, 86 |
|
Age group, years, n (%) |
|
|
|
|
<65 |
163 (45.8) |
121 (30.9) |
284 (38.0) |
|
≥65 |
193 (54.2) |
270 (69.1) |
463 (62.0) |
|
Race, n (%) |
|
|
|
|
White |
289 (81.2) |
295 (75.4) |
584 (78.2) |
|
Black or African American |
30 (8.4) |
61 (15.6) |
91 (12.2) |
|
Asian |
2 (0.6) |
10 (2.6) |
12 (1.6) |
|
Other* |
2 (0.6) |
4 (1.0) |
6 (0.8) |
|
Not reported |
33 (9.3) |
21 (5.4) |
54 (7.2) |
|
Ethnicity, n (%) |
|
|
|
|
Hispanic or Latino |
17 (4.8) |
18 (4.6) |
35 (4.7) |
|
Not Hispanic or Latino |
311 (87.4) |
342 (87.5) |
653 (87.4) |
|
Not reported |
28 (7.9) |
31 (7.9) |
59 (7.9) |
Source: Adapted from FDA Review
*Other includes American Indian or Alaska Native (3 patients), Native Hawaiian or Other Pacific Islander (2 patients), and Other (1 patient).
What are the benefits of this drug?
PET imaging done after POSLUMA injection showed sites of prostate-specific membrane antigen (PSMA) positive lesions in males with prostate cancer. PSMA is often present in prostate cancers.
What are the benefits of this drug (results of trials used to assess efficacy)?
Table 2 summarizes efficacy results for Trial 1 based on comparison of three blinded PET readers’ interpretation to pelvic lymph node histopathology results at the patient-level with hemipelvis region matching, such that at least one true positive hemipelvis region defines a true positive patient.
Table 2. Patient-Level, Hemipelvis Region-Matched Performance of POSLUMA PET for Detection of Pelvic Lymph Node Metastasis (N1) in Trial 1 (N=296)
|
Parameter |
Reader 1 |
Reader 2 |
Reader 3 |
|---|---|---|---|
|
True positive, n |
21 |
19 |
16 |
|
False positive, n |
16 |
14 |
7 |
|
True negative, n |
210 |
212 |
219 |
|
False negative, n |
49 |
51 |
54 |
|
Sensitivity, % (95% CI) |
30 (20, 42) |
27 (17, 39) |
23 (14, 35) |
|
Specificity, % (95% CI) |
93 (89, 96) |
94 (90, 97) |
97 (94, 99) |
|
Positive predictive value, % (95% CI) |
57 (40, 73) |
58 (39, 75) |
70 (47, 87) |
|
Negative predictive value, % (95% CI) |
81 (76, 86) |
81 (75, 85) |
80 (75, 85) |
Source: POSLUMA Prescribing Information
Sensitivity = (True positive/[True positive + False negative])
Specificity = (True negative/[True negative + False positive])
Abbreviations: CI, confidence interval; PET, positron emission tomography
For Trial 2, as a percentage of patients with an evaluable POSLUMA scan, 51% (95% CI: 46% to 56%) for reader 1, 48% (95% CI: 43% to 53%) for reader 2, and 49% (95% CI: 44% to 54%) for reader 3 had at least one matching positive region between the POSLUMA scan and either histopathology or other imaging. Of all POSLUMA-positive regions, 46% (95% CI: 42% to 50%) for reader 1, 60% (95% CI: 55% to 66%) for reader 2, and 53% (95% CI: 48% to 58%) for reader 3 were categorized as positive by either histopathology or other imaging.
Were there any differences in how well the drug worked in clinical trials among sex, race, and age groups?
- Sex: All trial participants were males; therefore, sex differences cannot be determined.
- Race: The majority of participants in the clinical trials were White. Differences among races could not be determined because of the small number of participants from other races.
- Age: POSLUMA worked similarly in patients younger and older than 65 years of age.
Were there any differences in how well the drug worked in clinical trials among sex, race, and age groups?
Table 3 summarizes efficacy results by age for Trial 1.
Table 3. Patient-Level Performance of POSLUMA PET for Detecting N1 Disease Compared to Surgical Pathology by Age for Trial 1 (Efficacy Analysis Population)
|
Parameter |
Reader 1 |
Reader 2 |
Reader 3 |
|---|---|---|---|
|
<65 years |
|
|
|
|
Sensitivity, n/N (%) |
12/36 (33.3) |
10/36 (27.8) |
9/36 (25.0) |
|
95% CI |
18.6, 51.0 |
14.2, 45.2 |
12.1, 42.2 |
|
Specificity, n/N (%) |
104/107 (97.2) |
102/107 (95.3) |
107/107 (100.0) |
|
95% CI |
92.0, 99.4 |
89.4, 98.5 |
96.6. 100.0 |
|
≥65 years |
|
|
|
|
Sensitivity, n/N (%) |
9/34 (26.5) |
9/34 (26.5) |
7/34 (20.6) |
|
95% CI |
12.9, 44.4 |
12.9, 44.4 |
8.7, 37.9 |
|
Specificity, n/N (%) |
106/119 (89.1) |
110/119 (92.4) |
112/119 (94.1) |
|
95% CI |
82.0, 94.1 |
86.1, 96.5 |
88.3, 97.6 |
Source: Clinical trial data
Sensitivity = (True positive/[True positive + False negative])
Specificity = (True negative/[True negative + False positive])
Abbreviations: CI = confidence interval
In Trial 2, there were no significant differences in efficacy when the data were stratified by age groups <65 years or ≥65 years.
What are the possible side effects?
POSLUMA is a radioactive drug and will contribute to a patient’s long-term cumulative radiation exposure.
The most common side effects of POSLUMA are diarrhea, blood pressure increase, and injection site pain occurring in fewer than 1 in 100 patients.
What are the possible side effects (results of trials used to assess safety)?
The safety of POSLUMA was evaluated in 747 patients with prostate cancer, each receiving one dose of POSLUMA. The adverse reactions reported in ≥0.4% of patients are shown in Table 4.
Table 4. Adverse Reactions in ≥0.4% of Patients With Prostate Cancer Receiving POSLUMA
|
Adverse Reaction |
Trial 1 N=356 n (%) |
Trial 2 N=391 n (%) |
Overall N=747 n (%) |
|---|---|---|---|
|
Diarrhea |
1 (0.3) |
4 (1.0) |
5 (0.7) |
|
Blood pressure increase |
1 (0.3) |
3 (0.8) |
4 (0.5) |
|
Injection site pain |
3 (0.8) |
0 |
3 (0.4) |
Source: Adapted from FDA Review
Were there any differences in side effects among sex, race, and age?
- Sex: All trial participants were males, therefore sex differences in side effects could not be determined.
- Race: The majority of participants in the clinical trials were White. The occurrence of common side effects among races could not be determined due to the low number of side effects in any racial group.
- Age: The occurrence of common side effects between patients younger and older than 65 years of age was similar.
Were there any differences in side effects of the clinical trials among sex, race, and age groups?
Adverse events by age group are presented in Table 5.
Table 5. Overview of Side Effects by Sex, Race, and Age in Trials BED-PSMA-301 and BED-PSMA-302, Safety Population
|
Trial 1 (BED-PSMA-301) POSLUMA N=356 |
Trial 2 (BED-PSMA-302) POSLUMA N=391 |
Overall POSLUMA N=747 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
|
Characteristic |
All Patients n (%) |
All Grades |
Grades 3 to 4 |
All Patients n (%) |
All Grades |
Grades 3 to 4 |
All Patients n (%) |
All Grades |
Grades 3 to 4 |
|
Sex, n (%) |
|
|
|
|
|
|
|
|
|
|
Male |
356 (100) |
28/356 (7.9) |
2/356 (0.6) |
391 (100) |
28/391 (7.2) |
4/391 (1.0) |
747 (100) |
56/747 (7.5) |
6/747 (0.8) |
|
Age group, years, n (%) |
|
|
|
|
|
|
|
|
|
|
<65 |
163 (45.8) |
14/163 (8.6) |
0/163 (0) |
121 (30.9) |
11/121 (9.1) |
1/121 (0.8) |
284 (38.0) |
25/284 (8.8) |
1/284 (0.4) |
|
≥65 |
193 (54.2) |
14/193 (7.3) |
2/193 (1.0) |
270 (69.1) |
17/270 (6.3) |
3/270 (1.1) |
463 (62.0) |
31/463 (6.7) |
5/463 (1.1) |
|
Race, n (%) |
|
|
|
|
|
|
|
|
|
|
White |
289 (81.2) |
22/289 (7.6) |
2/289 (0.7) |
295 (75.4) |
21/295 (7.1) |
2/295 (0.7) |
584 (78.2) |
43/584 (7.4) |
4/584 (0.7) |
|
Black or African American |
30 (8.4) |
2/30 (6.7) |
0/30 (0) |
61 (15.6) |
5/61 (8.2) |
2/61 (3.3) |
91 (12.2) |
7/91 (7.7) |
2/91 (2.2) |
|
Asian |
2 (0.6) |
0/2 (0) |
0/2 (0) |
10 (2.6) |
0/10 (0) |
0/10 (0) |
12 (1.6) |
0/12 (0) |
0/12 (0) |
|
Other |
1 (0.3) |
1/1 (100) |
0/1 (0) |
0 (0) |
0/0 (NA) |
0/0 (NA) |
1 (0.1) |
1/1 (100) |
0/1 (0) |
|
Not Reported |
33 (9.3) |
3/33 (9.1) |
0/33 (0) |
21 (5.4) |
2/21 (9.5) |
0/21 (0) |
54 (7.2) |
5/54 (9.3) |
0/54 (0) |
|
Native Hawaiian or Other Pacific Islander |
1 (0.3) |
0/1 (0) |
0/1 (0) |
1 (0.3) |
0/1 (0) |
0/1 (0) |
2 (0.3) |
0/2 (0) |
0/2 (0) |
|
American Indian or Alaska Native |
0 (0) |
0/0 (NA) |
0/0 (NA) |
3 (0.8) |
0/3 (0) |
0/3 (0) |
3 (0.4) |
0/3 (0) |
0/3 (0) |
Table 5. Overview of Side Effects by Sex, Race, and Age in Trials BED-PSMA-301 and BED-PSMA-302, Safety Population
Source: adae.xpt (eCTD seq 0006); FDA reviewer's analysis
Abbreviation: N, number of patients in the safety population; n, number of patients with given characteristic; Ns, total number of patients in each category
GLOSSARY
CLINICAL TRIAL: Voluntary research studies conducted in people and designed to answer specific questions about the safety or effectiveness of drugs, vaccines, other therapies, or new ways of using existing treatments.
COMPARATOR: A previously available treatment or placebo used in clinical trials that is compared to the actual drug being tested.
EFFICACY: How well the drug achieves the desired response when it is taken as described in a controlled clinical setting, such as during a clinical trial.
PLACEBO: An inactive substance or “sugar pill” that looks the same as, and is given the same way as, an active drug or treatment being tested. The effects of the active drug or treatment are compared to the effects of the placebo.
SUBGROUP: A subset of the population studied in a clinical trial. Demographic subsets include sex, race, and age groups.