2021 FDA Science Forum
Cardiac Contractility Modulation Stimulation During Systole Enhances Contraction and Calcium Handling Properties in Human-Induced Pluripotent Stem Cell -Derived Cardiomyocytes
- Authors:
- Center:
-
Contributing OfficeCenter for Devices and Radiological Health
Abstract
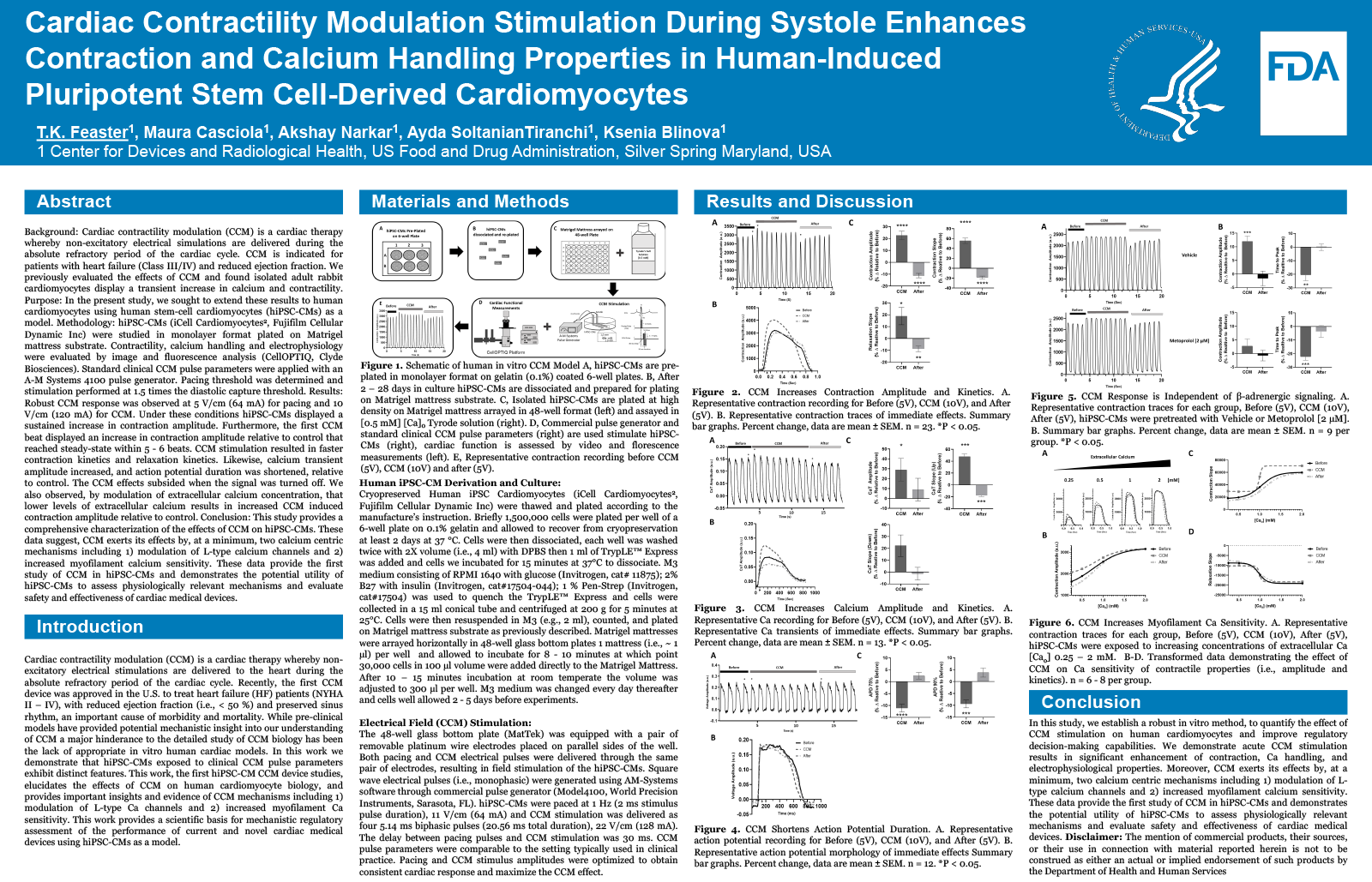
Background
Cardiac contractility modulation (CCM) is a cardiac therapy whereby non-excitatory electrical simulations are delivered during the absolute refractory period of the cardiac cycle. CCM is indicated for patients with heart failure (Class III/IV) and reduced ejection fraction. We previously evaluated the effects of CCM and found isolated adult rabbit cardiomyocytes display a transient increase in calcium and contractility.
Purpose
In the present study, we sought to extend these results to human cardiomyocytes using human stem-cell cardiomyocytes (hiPSC-CMs) as a model.
Methodology
hiPSC-CMs (iCell Cardiomyocytes2, Fujifilm Cellular Dynamic Inc) were studied in monolayer format plated on Matrigel mattress substrate. Contractility, calcium handling and electrophysiology were evaluated by image and fluorescence analysis (CellOPTIQ, Clyde Biosciences). Standard clinical CCM pulse parameters were applied with an A-M Systems 4100 pulse generator. Pacing threshold was determined and stimulation performed at 1.5 times the diastolic capture threshold.
Results
Robust CCM response was observed at 5 V/cm (64 mA) for pacing and 10 V/cm (120 mA) for CCM. Under these conditions hiPSC-CMs displayed a sustained increase in contraction amplitude. Furthermore, the first CCM beat displayed a 19.7±0.03 %, (**P<0.01, n=10) increase in contraction amplitude relative to control that reached steady-state within 5 - 6 beats at 8.3±0.16 %. CCM stimulation resulted in faster contraction kinetics (i.e., time to peak 90%) and relaxation kinetics (i.e., time to baseline 90%) of 25.9±0.07 % and 18.6±0.07 % respectively. Likewise, calcium transient amplitude increased by 59.3±0.03% (*P<0.05, n=3) relative to control. The CCM effects subsided when the signal was turned off. We also observed, by modulation of extracellular calcium concentration, that lower levels of extracellular calcium results in increased CCM induced contraction amplitude relative to control.
Conclusion
This study provides a comprehensive characterization of the effects of CCM on hiPSC-CMs. These data suggest, CCM exerts its effects by, at a minimum, two calcium centric mechanisms including 1) modulation of L-type calcium channels and 2) increased myofilament calcium sensitivity. These data provide the first study of CCM in hiPSC-CMs and demonstrates the potential utility of hiPSC-CMs to assess physiologically relevant mechanisms and evaluate safety and effectiveness of cardiac medical devices.
Disclaimer
The mention of commercial products, their sources, or their use in connection with material reported herein is not to be construed as either an actual or implied endorsement of such products by the Department of Health and Human Services