Ensuring the Rigor of Regulatory Science: CDER Conducts Laboratory and Clinical Studies to Investigate Reports of NDMA Production from Ingested Ranitidine Products
Ranitidine, which blocks histamine-induced acid secretion in the stomach, was approved in 1983. It became widely used over the ensuing decades as a prescription and over-the-counter product. In 2019, the FDA received a citizen petition indicating that high levels of N-nitrosodimethylamine (NDMA), a probable human carcinogen, were detected in specific ranitidine products. The petitioner also proposed that ranitidine could convert to NDMA in humans. In response, the FDA immediately alerted the public, and CDER scientists worked quickly to mobilize specialized FDA laboratory and clinical research capabilities.
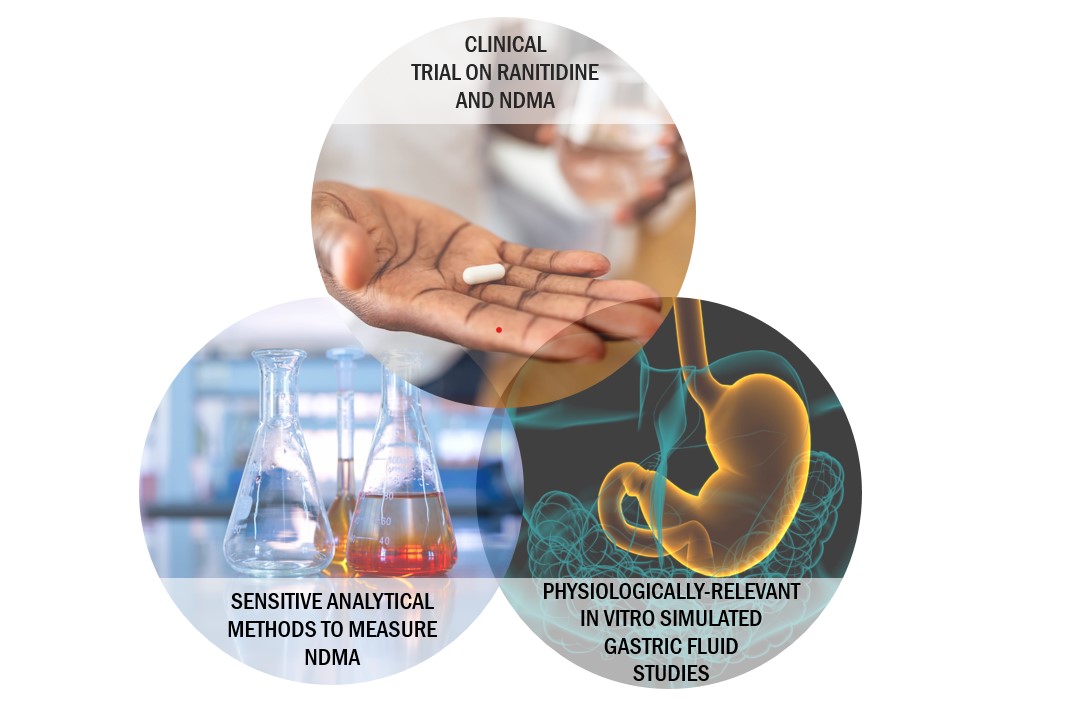
CDER’s initial research focused on assessing the amount of NDMA in ranitidine drug products. CDER researchers found that the procedures previously used to quantify NDMA were not appropriate for assessing its presence in ranitidine, owing to the use of high temperatures that could convert ranitidine to NDMA during that analysis. CDER researchers therefore developed and validated low-temperature analytical methods and found that the amounts of NDMA contained in ranitidine products were 3,000-fold lower than those reported in the citizen petition; however, these lower amounts of NDMA were still above the FDA-acceptable level, corresponding to a daily intake limit of 96 ng NMDA per day, in many of the ranitidine lots tested. CDER scientists further observed that the amounts of NDMA in ranitidine samples could increase over time, prompting the FDA to request the market withdrawal of ranitidine products. The agency noted, however, that if ranitidine products could be manufactured to control NDMA amounts, they could be allowed back on the market—but additional information would first be needed to understand whether NDMA could form in vivo from ranitidine in humans.
Assessing the Potential for Ranitidine to Convert to NDMA in Humans
The citizen petition referenced in vitro studies suggesting ranitidine could convert to NDMA in simulated gastric fluid (with high levels of supplemental nitrite) and a prior clinical study with 10 participants. The referenced clinical study reported an approximate 400-fold increase in NDMA excreted in urine over 24-hours after oral ranitidine 150 mg. However, there were multiple limitations to the referenced study, including the lack of placebo-controlled randomization; the lack of information concerning environmental or dietary exposure of study participants to NDMA or the reactants that may contribute to NDMA production; and a lack of detail about biological sample handling and validation of analytical methods.
To better address the possibility of NDMA production from ranitidine in humans, CDER scientists conducted a more rigorous, randomized, double-blinded, placebo-controlled clinical trial, published in JAMA: Journal of the American Medical Association. The study included 18 participants who each received ranitidine (300 mg) and placebo on two different diets, the second of which was designed to contain higher amounts of nitrites, nitrates, and NDMA from foods such as cured meats. The study used rigorous procedures for handling urine and blood samples and validated low-temperature analytical methods for measuring NDMA. The CDER researchers found no evidence of elevated NDMA content in the urine of participants over the 24 hours after they took ranitidine, regardless of diet. CDER’s clinical trial further found that ranitidine did not increase NDMA in blood plasma and did not increase dimethylamine (DMA) (proposed in the citizen petition to be the precursor to NDMA generated from ranitidine) in plasma or urine.
In addition, CDER researchers conducted an in vitro study, also published by the JAMA network, on the potential for ranitidine to convert to NDMA in simulated gastric fluid. Importantly, CDER researchers performed an assessment of the range of physiologic gastric nitrite concentrations from prior clinical studies, which had not been done in a recent prior study published in the same journal. CDER researchers found that ranitidine did not produce NDMA in simulated gastric fluid unless nitrite was 50-fold greater than the upper range of physiologic gastric nitrite concentration in acidic conditions. The combined findings from CDER’s in vivo clinical trial and in vitro experiments do not support the conclusion that ranitidine is converted to NDMA in humans.
Broader Context of CDER’s Research Findings
After CDER completed its clinical trial and submitted the results for publication, the prior clinical study that had reported a 400-fold increase in NDMA urinary excretion after ingestion of ranitidine was retracted by the authors, citing that an analytical artifact may have contributed to their results. In addition, as summarized in the reports that CDER investigators published in JAMA and JAMA Network Open, other reports of nonclinical results (or commentaries on nonclinical studies) had described in vitro findings without properly contextualizing the physiological relevance of their test conditions. Indeed, the CDER in vitro analysis demonstrates that proper investigation into the potential for drugs to lead to NDMA formation in humans should include physiologically relevant conditions.
As noted above and elsewhere, ranitidine products were removed from the US market in April 2020, owing to unacceptable amounts of NDMA in ranitidine products that could increase over time; however, the product approvals were not withdrawn, and the FDA may consider allowing ranitidine products back on the market if they are proven to be stable, with low, acceptable amounts of NDMA that do not increase over time during storage. All FDA-approved drug products must meet FDA standards for safety, effectiveness, and quality before they are allowed on the market. In addition, it may be assuring to patients and health care professionals to consider in proper context the potential risk posed by products that may contain NDMA amounts at the acceptable daily limit; the cancer risk for an average individual with a mass of 50 kg and consuming 96 ng of NDMA daily for 70 years is 1 in 100,000.
CDER Research to Address Emergent Regulatory and Public Health Questions
CDER’s research capabilities and activities empower the agency to respond rapidly to emergent regulatory and public health questions regarding the products it regulates. In the case discussed above, CDER developed new analytical methods for measuring NDMA in drug products and in biological fluids, and then conducted rigorous laboratory and clinical studies. The findings suggested that prior reports had detected falsely high levels of NDMA in ranitidine drug products and human biological fluids.
In another case, pertaining to sunscreens (also a type of widely used over-the-counter product), historical assumptions had posited that the active ingredients in sunscreens were not absorbed; however, the studies necessary for addressing this absorption issue were not pursued until CDER regulatory science initiatives led the way. CDER scientists conducted both laboratory and clinical research, including 2 clinical trial reports published in JAMA (report 1 and report 2), that demonstrated that sunscreen active ingredients in fact can be absorbed, revealing the need for further studies by industry.
In these and many other cases (see, for example, CDER’s Impact Stories or the CDER Division of Applied Regulatory Science annual report), CDER scientists play a unique role in moving new science into the drug regulatory review process and addressing emergent regulatory and public health questions.
The Spotlight series presents generalized perspectives on ongoing research- and science-based activities within CDER. Spotlight articles should not be construed to represent FDA’s views or policies.
References to Published CDER Investigations
Florian J, Matta MK, DePalma R, Gershuny V, Patel V, Hsiao CH, Zusterzeel R, Rouse R, Prentice K, Nalepinski CG, Kim I, Yi S, Zhao L, Yoon M, Selaya S, Keire D, Korvick J, Strauss DG. Effect of Oral Ranitidine on Urinary Excretion of N-Nitrosodimethylamine (NDMA): A Randomized Clinical Trial. JAMA. 2021 Jun 28. doi: 10.1001/jama.2021.9199.
Gao Z, Karfunkle M, Ye W, Marzan TA, Yang J, Lex T, Sommers C, Rodriguez JD, Han X, Florian J, Strauss DG, Keire DA. In Vitro Analysis of N-Nitrosodimethylamine (NDMA) Formation From Ranitidine Under Simulated Gastrointestinal Conditions. JAMA Netw Open. 2021 Jun 1;4(6):e2118253. doi: 10.1001/jamanetworkopen.2021.18253.