Drug Trials Snapshots: RINVOQ
HOW TO USE THIS SNAPSHOT
The information provided in Snapshots highlights who participated in the clinical trials that supported the FDA approval of this drug, and whether there were differences among sex, race and age groups. The “MORE INFO” bar shows more detailed, technical content for each section. The Snapshot is intended as one tool for consumers to use when discussing the risks and benefits of the drugs.
LIMITATIONS OF THIS SNAPSHOT:
Do not rely on Snapshots to make decisions regarding medical care. Always speak to your health provider about the risks and benefits of a drug. Refer to the RINVOQ Package Insert for complete information.nter text
RINVOQ (upadacitinib)
RIN-voke
AbbVie Inc
Approval date: August 16, 2019
DRUG TRIALS SNAPSHOT SUMMARY:
What is the drug for?
RINVOQ is a drug used to treat adult patients with moderately to severely active rheumatoid arthritis (RA) in whom methotrexate [(MTX)a drug used to treat active arthritis] did not work well or could not be tolerated.
How is this drug used?
RINVOQ is a tablet that is taken once daily by mouth.
What are the benefits of this drug?
In the clinical trials, a greater proportion of patients who received RINVOQ achieved an improvement in the signs and symptoms of RA in comparison to patients who received comparator drug or placebo.
What are the benefits of this drug (results of trials used to assess efficacy)?
The table below summarizes the efficacy results for individual trials 2 to 5. The primary endpoint was the proportion of patients who achieved an ACR20 response.
Table 2. Difference Between RINVOQ and Control for Percent ACR20 Responders
|
Trial |
Control Treatment |
Background Disease Modifying Treatments |
Treatment Difference |
|
|
|
|
|
Difference |
95% CI |
|
Trial 2a,d |
methotrexate |
|
26% |
(17%, 36%) |
|
Trial 3b |
Placebo |
cDMARDs, methotrexate1 |
28% |
(19%, 37%) |
|
Trial 4a |
Placebo |
methotrexate |
34% |
(29%, 39%) |
|
Trial 5c |
Placebo |
cDMARDs, methotrexate1 |
36% |
(26%, 46%) |
1. conventional disease-modifying anti-rheumatic drugs and/or methotrexate
a. Patients with prior inadequate response to methotrexate
b. Patients with prior inadequate response to cDMARDs and/or methotrexate
c. Patients with prior inadequate response to biologic disease-modifying anti-rheumatic drugs
d. Patients who discontinued treatment or were missing data at week of evaluation had their ACR20 outcome imputed as non-response in the analyses.
cDMARDS = conventional disease-modifying anti-rheumatic drugs
FDA Review
Were there any differences in how well the drug worked in clinical trials among sex, race and age?
- Sex: RINVOQ worked similarly in men and women.
- Race: RINVOQ worked similarly in White, Black or African American, and Asian races.
- Age: RINVOQ worked similarly in all age groups tested (younger than 40 years of age, 40 to 64 years of age, and 65 years of age and older).
Were there any differences in how well the drug worked in clinical trials among sex, race, and age groups?
The tables below summarize subgroup results based on the primary endpoint analyses for RINVOQ alone compared to methotrexate alone and RINVOQ compared to placebo in combination with DMARD/MTX respectively.
Table 3. Effects of RINVOQ on Percent ACR20 Responders at Week 14 by Subgroups-Methotrexate Controlled Trial
|
Demographic Parameter |
ACR20 % (n/N) |
Treatment Differencea |
|
|---|---|---|---|
|
|
Methotrexate |
RINVOQ |
(95% CI) |
|
Sex |
|||
|
Men |
43% (16/37) |
60% (26/43) |
21% (2%, 40%) |
|
Women |
41% (73/179) |
70% (121/174) |
28% (18%, 38%) |
|
Race |
|||
|
White |
43% (76/176) |
68% (118/173) |
26% (16%, 35%) |
|
Black or African American |
45% (5/11) |
33% (5/15) |
6% (-32%, 43%) |
|
Asian |
29% (7/24) |
88% (21/24) |
51% (27%, 75%) |
|
Age Group (years) |
|||
|
Less than 40 |
52% (12/23) |
82% (23/28) |
27% (10%, 45%) |
|
40 to 64 |
39% (58/148) |
68% (100/147) |
28% (18%, 38%) |
|
65 or Older |
42% (19/45) |
57% (24/42) |
21% (4%, 38%) |
a Treatment differences and credible intervals may not match value of (treatment - control) since estimates include relevance of outcomes from other subgroups. Patients who discontinued treatment or were missing data at week of evaluation had their ACR20 outcome imputed as non-response in the analyses.
FDA Statistical Review
Table 4. Effects of RINVOQ on Percent ACR20 Responders at Week 12 by Subgroups-Pooled Placebo Controlled Trials 1
|
Demographic Parameter |
ACR20 % (n/N) |
Treatment Differencea |
|
|
|
Placebo |
RINVOQ |
(95% CI) |
|
Sex |
|||
|
Men |
37% (82/220) |
68% (133/196) |
31% (23%, 40%) |
|
Women |
34% (282/821) |
68% (573/840) |
34% (29%, 38%) |
|
Race |
|||
|
White |
36% (324/891) |
70% (631/906) |
33% (29%, 37%) |
|
Black or African American |
17% (12/69) |
48% (30/63) |
32% (21%, 44%) |
|
Asian |
33% (21/63) |
71% (37/52) |
35% (23%, 47%) |
|
Age Group (years) |
|||
|
Younger than 40 |
49% (62/126) |
68% (78/115) |
23% (11%, 35%) |
|
40 to 64 |
32% (222/688) |
68% (480/707) |
35% (30%, 40%) |
|
65 or Older |
35% (80/227) |
69% (148/214) |
33% (25%, 41%) |
1 Pooled trials included trials 3, 4, and 5.
a Treatment differences and credible intervals may not match values of (treatment - control) since estimates include relevance of outcomes from other subgroups.
Patients who discontinued treatment or were missing data at week of evaluation had their ACR20 outcome imputed as non-response in the analyses.
FDA Statistical Review
What are the possible side effects?
RINVOQ may cause serious side effects including;
- life threatening infections that may lead to hospitalization or death,
- increased risk of lymphoma (immune system cancer) and some other cancers and
- blood clots in the veins and arteries.
Other serious side effects include tears in the stomach or intestines, low blood cell counts, abnormal liver tests, harm to a fetus, and increased cholesterol.
The most common side effects are upper respiratory infections, nausea, cough, and fever.
What are the possible side effects (results of trials used to assess safety)?
Below is the summary of the most common adverse reactions observed in patients treated with RINVOQ or placebo.
Table 5. Adverse Reactions Reported in greater than or equal to 1% of Rheumatoid Arthritis Patients Treated with RINVOQ 15 mg in Placebo-controlled Trials
|
Adverse Reaction |
RINVOQ |
Placebo |
|
n=1035 |
n=1042 |
|
|
Upper respiratory tract infection (URTI)* |
13.5 |
9.5 |
|
Nausea |
3.5 |
2.2 |
|
Cough |
2.2 |
1.0 |
|
Pyrexia |
1.2 |
0 |
|
*URTI includes: acute sinusitis, laryngitis, nasopharyngitis, oropharyngeal pain, pharyngitis, pharyngotonsillitis, rhinitis, sinusitis, tonsillitis, viral upper respiratory tract infection |
||
Patients from Trials 3-5 were included.
RINVOQ Prescribing Information
Were there any differences in side effects among sex, race and age?
- Sex: The occurrence of side effects was similar in men and women.
- Race: The occurrence of side effects was similar among races.
- Age: The occurrence of side effects increased with age.
Were there any differences in side effects of the clinical trials among sex, race, and age groups?
The table below summarizes the occurrence of adverse events by subgroups.
Table 6. Subgroup Analysis of Adverse Events
|
Demographic Characteristic |
RINVOQ |
Placebo |
|
Sex |
|
|
|
Men |
100/196 (51) |
101/220 (46) |
|
Women |
480/839 (57) |
403/822 (49) |
|
Race |
||
|
White |
498/905 (55) |
420/892 (47) |
|
Black |
40/63 (63) |
40/69 (58) |
|
Asian |
34/52 (65) |
35/63 (55) |
|
American Indian or Alaska Native |
0/4 (0) |
1/3 (33) |
|
Native Hawaiian or Other Pacific Islander |
0/0 (0) |
0/1 (0) |
|
Other |
8/11 (73) |
8/14 (57) |
|
Age Group |
||
|
< 65 years |
466/821 (57) |
401/815 (49) |
|
65 - 74 years |
93/181 (51) |
86/189 (45) |
|
> 75 years |
21/33 (64) |
17/38 (45) |
Patients from Trials 3-5 were included.
Clinical Trial Data
WHO WAS IN THE CLINICAL TRIALS?
Who participated in the clinical trials?
The FDA approved RINVOQ based on evidence from five clinical trials (Trial 1/NCT02706873, Trial 2/NCT02706951, Trial 3/NCT02675426, Trial 4/NCT02629159, Trial 5/NCT02706847) of 3,141 patients with active rheumatoid arthritis (RA). The trials were conducted in Australia, New Zealand, Israel, South Africa, Asia, North/Central/South America, and Europe.
Demographics of the population that provided data for the assessment of side effects (safety population) are described in Table 8.
The figure below summarizes how many men and women were in the clinical trials.
Figure 1. Baseline Demographics by Sex
FDA Review
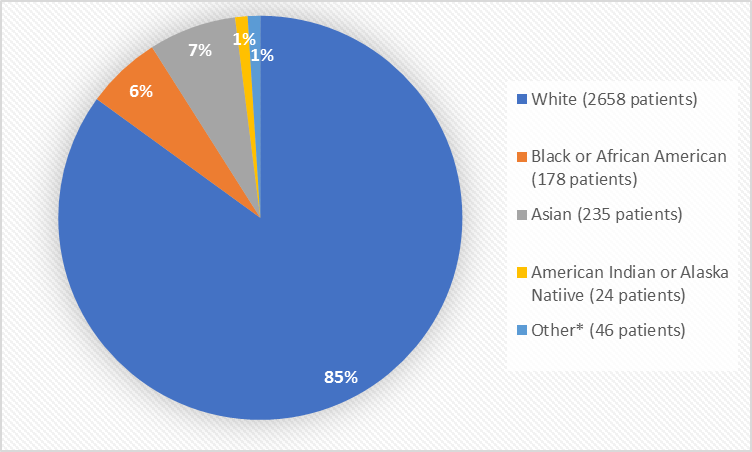
Figure 2 and Table 1 summarize the percentage of patients by race in the clinical trials.
Figure 2. Baseline Demographics by Race
*Other includes Native Hawaiian or Other Pacific Islander
FDA Review
Table 1. Demographics of Efficacy Trials by Race
|
Race |
Number of Patients |
Percentage of Patients |
|---|---|---|
|
White |
2658 |
85% |
|
Black or African American |
178 |
6% |
|
Asian |
235 |
7% |
|
American Indian or Alaska Native |
24 |
1% |
|
Native Hawaiian or Other Pacific Islander |
6 |
Less than 1% |
|
Other |
40 |
1% |
FDA Review
Figure 3 summarizes the percentage of patients by race in the clinical trials used to evaluate efficacy.
Figure 3. Baseline Demographics by Age
FDA Review
The table below summarize demographics of patients in the efficacy (Table 7) and safety (Table 8) populations.
Table 7. Trial Demographics
|
Demographic Characteristics |
RINVOQ |
MTX |
Placebo |
Total |
|
Sex |
||||
|
Men |
315 (20%) |
111 (21%) |
220 (21%) |
646 (21%) |
|
Women |
1255 (80%) |
419 (79%) |
821 (79%) |
2495 (79%) |
|
Race |
||||
|
White |
1335 (85%) |
432 (82%) |
891 (86%) |
2658 (85%) |
|
Black or African American |
86 (5%) |
23 (4%) |
69 (7%) |
178 (6%) |
|
Asian |
111 (7%) |
61 (12%) |
63 (6%) |
235 (7%) |
|
American Indian or Alaska Native |
16 (1%) |
5 (1%) |
3 (<1%) |
24 (1%) |
|
Native Hawaiian or Other Pacific Islander |
3 (<1%) |
2 (<1%) |
1 (<1%) |
6 (<1%) |
|
Other |
19 (1%) |
7 (1%) |
14 (1%) |
40 (1%) |
|
Age Group |
||||
|
<40 |
203 (13%) |
73 (14%) |
126 (12%) |
402 (13%) |
|
40 - 64 |
1058 (67%) |
354 (67%) |
688 (66%) |
2100 (67%) |
|
>65 |
309 (20%) |
103 (19%) |
227 (22%) |
639 (20%) |
|
Ethnicity |
|
|
|
|
|
Hispanic |
431 (27%) |
152 (29%) |
257 (25%) |
840 (27%) |
|
Non-Hispanic |
1139 (73%) |
378 (71%) |
784 (75%) |
2301 (73%) |
|
Region |
||||
|
United States |
406 (26%) |
102 (19%) |
312 (30%) |
820 (26%) |
|
North America Excluding United States |
25 (2%) |
8 (1%) |
9 (1%) |
42 (1%) |
|
South/Central America |
304 (19%) |
121 (23%) |
181 (17%) |
606 (19%) |
|
Europe |
660 (42%) |
209 (39%) |
451 (43%) |
1320 (42%) |
|
Asia |
92 (6%) |
54 (10%) |
37 (3%) |
183 (6%) |
|
Rest of the World |
83 (5%) |
36 (7%) |
51 (5%) |
170 (5%) |
FDA Review
Table 8. Demographics of Safety Population
|
Demographic Characteristics |
RINVOQ |
Placebo |
Total |
|
Sex |
|||
|
Men |
196 (19%) |
220 (21%) |
416 (40%) |
|
Women |
839 (81%) |
822 (79%) |
1661 (80%) |
|
Race |
|||
|
White |
905 (87%) |
892 (86%) |
1797 (86%) |
|
Black or African American |
63 (6%) |
69 (7%) |
132 (6%) |
|
Asian |
52 (5%) |
63 (6%) |
115 (5%) |
|
American Indian or Alaska Native |
4 (<1%) |
3 (<1%) |
7 (<1%) |
|
Native Hawaiian or Other Pacific Islander |
0 |
1 (<1%) |
1 (<1%) |
|
Other |
11 (1%) |
14 (1%) |
25 (1%) |
|
Age Group |
|||
|
<40 |
115 (11%) |
126 (12%) |
241 (12%) |
|
40 - 64 |
706 (68%) |
689 (66%) |
1395 (67%) |
|
>65 |
214 (21%) |
227 (22%) |
441 (21%) |
|
Ethnicity |
|
|
|
|
Hispanic |
273 (26%) |
257 (25%) |
530 (25%) |
|
Non-Hispanic |
762 (74%) |
785 (75%) |
1547 (75%) |
|
Region |
|||
|
North America |
319 (31%) |
321 (31%) |
640 (31%) |
|
Others |
183 (18%) |
181 (17%) |
364 (17%) |
|
Europe |
448 (43%) |
452 (43%) |
900 (43%) |
|
Asia |
38 (4%) |
37 (4%) |
75 (4%) |
|
Rest of the World |
47 (4%) |
51 (5%) |
98 (5%) |
Clinical Trial Data
How were the trials designed?
Five trials established the benefits and side effects of RINVOQ. Trials enrolled patients with moderate to severe active RA in whom disease-modifying antirheumatic drugs (DMARDS) did not work well or could not be tolerated. All patients had at least 6 tender and 6 swollen joints, and increased levels of high sensitivity C-reactive protein (hsCRP). hsCRP is a substance produced by the body to protect itself from illness. Trials lasted up to 5 years.
Trial 1 enrolled patients who had never been treated with MTX. Patients were randomly assigned to receive one of two doses of RINVOQ or MTX daily for 24 weeks. Neither the patient nor the healthcare providers knew which medication was being given until after this 24-week treatment period.
Trial 2 enrolled patients in whom MTX did not work well. Patients were randomly assigned to receive one of two doses of RINVOQ daily by mouth or continue their usual dose of MTX for 14 weeks. At Week 14, patients who were assigned to MTX received RINVOQ by mouth daily. Neither the patient nor the healthcare providers knew which medication was being given.
Trial 3 enrolled patients in whom DMARDS did not work well. Patients were randomly assigned to receive one of two doses of RINVOQ or placebo daily by mouth in addition to DMARDS for 12 weeks. At Week 12, patients who received placebo were re-assigned to RINVOQ daily. Neither the patient nor the healthcare providers knew which medication was being given.
Trial 4 enrolled patients in whom MTX did not work well. Patients were randomly assigned to receive RINVOQ or placebo daily by mouth in addition to MTX for 14 weeks. Patients receiving placebo who did not have adequate improvement of signs and/or symptoms could be switched to RINVOQ after Week 14. At Week 26, all patients receiving placebo were switched to RINVOQ once daily by mouth. Neither the patient nor the healthcare providers knew which medication was being given.
Trial 5 enrolled patients in whom DMARDS did not work well or could not be tolerated. Patients were randomly assigned to receive one of two doses of RINVOQ or placebo treatment daily added to DMARDs for 12 weeks. At Week 12, patients who received placebo were re-assigned to RINVOQ daily.
The benefit of RINVOQ was measured by comparing the proportion of patients treated with RINVOQ who achieved an American College of Rheumatology 20 (ACR20) response at Week 12 or Week 14 to the proportion of patients treated with MTX or placebo who achieved an ACR20 response. ACR20 is a 20% improvement in signs and symptoms of RA.
How were the trials designed?
The efficacy and safety of RINVOQ was evaluated in five randomized, double-blind, placebo- and active-controlled trials of patients with moderately to severely active RA.
In Trial 1, patients who were naïve to MTX. Patients received RINVOQ or MTX orally as once daily monotherapy. The primary endpoint was the proportion of patients who achieved an ACR50 response at Week 12.
In Trial 2, patients who had an inadequate response to MTX received RINVOQ 15 mg or a non-recommended dose of RINVOQ once daily orally as monotherapy or continued their stable dose of MTX oral monotherapy daily. At Week 14, patients who were randomized to MTX were advanced to RINVOQ 15 mg or a non-recommended dose of RINVOQ once daily monotherapy in a blinded manner based on pre-determined assignment at baseline. The primary endpoint was the proportion of patients who achieved an ACR20 response at Week 14. The ACR20 is a composite measure defined as both improvement of 20% in the number of tender and number of swollen joints, and a 20% improvement in three of the following five criteria: patient global assessment, physician global assessment, functional ability measure, visual analog pain scale, and acute phase reactant (erythrocyte sedimentation rate or C-reactive protein).
In Trial 3, patients who had an inadequate response to conventional disease modifying anti-rheumatic drugs (cDMARDs) received oral RINVOQ 15 mg, a non-recommended dose of oral RINVOQ once daily or placebo added to background cDMARD therapy once daily. At Week 12, patients who were randomized to placebo were advanced to RINVOQ 15 mg or a non-recommended dose of oral RINVOQ once daily in a blinded manner based on pre-determined assignment at baseline. The primary endpoint was the proportion of patients who achieved an ACR20 response at Week 12.
In Trial 4, patients who had an inadequate response to MTX received RINVOQ 15 mg orally once daily with matching placebo injection every two weeks, active comparator injection every two weeks with matching placebo tablet orally once daily, or placebo once daily and matching placebo injection every two weeks added to background MTX. From Week 14, non-responding patients on RINVOQ 15 mg could be rescued to active comparator in a blinded manner, and non-responding patients on active comparator or placebo could be rescued to RINVOQ 15 mg in a blinded manner. At Week 26, all patients randomized to placebo were switched to RINVOQ 15 mg once daily in a blinded manner. The primary endpoint was the proportion of patients who achieved an ACR20 response at Week 12 versus placebo.
In Trial 5, patients who had an inadequate response or intolerance to biologic DMARDs received RINVOQ 15 mg or a non-recommended dose of RINVOQ once daily or placebo added to background cDMARD therapy once daily. At Week 12, patients who were randomized to placebo were advanced to RINVOQ 15 mg or a non-recommended dose of RINVOQ once daily in a blinded manner based on pre-determined assignment at baseline. The primary endpoint was the proportion of patients who achieved an ACR20 response at Week 12.
GLOSSARY
CLINICAL TRIAL: Voluntary research studies conducted in people and designed to answer specific questions about the safety or effectiveness of drugs, vaccines, other therapies, or new ways of using existing treatments.
COMPARATOR: A previously available treatment or placebo used in clinical trials that is compared to the actual drug being tested.
EFFICACY: How well the drug achieves the desired response when it is taken as described in a controlled clinical setting, such as during a clinical trial.
PLACEBO: An inactive substance or “sugar pill” that looks the same as, and is given the same way as, an active drug or treatment being tested. The effects of the active drug or treatment are compared to the effects of the placebo.
SUBGROUP: A subset of the population studied in a clinical trial. Demographic subsets include sex, race, and age groups.