Drug Trial Snapshot: TEGSEDI
HOW TO USE THIS SNAPSHOT
The information provided in Snapshots highlights who participated in the clinical trials that supported the FDA approval of this drug, and whether there were differences among sex, race and age groups. The “MORE INFO” bar shows more detailed, technical content for each section. The Snapshot is intended as one tool for consumers to use when discussing the risks and benefits of the drugs.
LIMITATIONS OF THIS SNAPSHOT:
Do not rely on Snapshots to make decisions regarding medical care. Always speak to your health provider about the risks and benefits of a drug. Refer to the TEGSEDI Package Insert for complete information.
TEGSEDI (inotersen)
teg-SED-ee
Ionis Pharmaceuticals, Inc.
Approval date:October 5, 2018
DRUG TRIALS SNAPSHOT SUMMARY:
What is the drug for?
TEGSEDI is a drug for the treatment of nerve damage in adult patients with hereditary transthyretin-mediated amyloidosis. Transthyretin-mediated amyloidosis is the buildup of abnormal deposits of a substance called amyloid in the body's organs and tissues. Amyloid disrupts the function of organs and tissues.
How is this drug used?
TEGSEDI is injected under the skin (a subcutaneous injection) once weekly.
What are the benefits of this drug?
Compared to patients receiving placebo injections, patients who received TEGSEDI had fewer symptoms of nerve damage, as well as better muscle strength and reflexes.
What are the benefits of this drug (results of trials used to assess efficacy)?
The table below summarizes clinical efficacy results for the clinical trial. The co-primary efficacy endpoints were the change from baseline to Week 66 in the modified Neuropathy Impairment Score +7 (mNIS+7) and the Norfolk Quality of Life Diabetic Neuropathy (QoL-DN) total score. Higher scores represent greater severity of disease.
Table 2. Clinical Efficacy Results
|
Endpoint |
Baseline |
Change from Baseline to Week 66 (LS Mean) |
TEGSEDI – placebo Treatment Difference LS Mean |
p- value |
||
|---|---|---|---|---|---|---|
|
TEGSEDI |
Placebo |
TEGSEDI |
Placebo |
|||
|
Primarya |
||||||
|
mNIS+7b, c |
80.2(38.2) |
75.3 (39.4) |
5.8 (2.1) |
25.5 (2.7) |
-19.7 |
<0.001 |
|
Norfolk QOL-DNb, d |
48.7(26.6) |
48.7(27.2) |
1.0(2.1) |
12.7(2.7) |
-11.7 |
<0.001 |
CI, confidence interval; LS, least squares; mNIS, modified Neuropathy Impairment Score; QoL-DN,Quality of Life – Diabetic Neuropathy
a All endpoints analyzed using the mixed-effect model repeated measures (MMRM) method.
b A lower value indicates less impairment/fewer symptoms.
c The primary analysis population for the mNIS+7 analysis included N=95 TEGSEDI patients and N=56 placebo patients
d The primary analysis population for the Norfolk QOL-DN analysis included N=94 TEGSEDI patients and N=57 placebo patients.
TEGSEDI Prescribing Information
Were there any differences in how well the drug worked in clinical trials among sex, race and age?
- Sex: TEGSEDI worked similarly in males and females.
- Race: The majority of patients in the trial was White. Differences in how well the drug worked among races could not be determined because of the small number of patients in other races.
- Age: TEGSEDI worked similarly in patients younger and older than 65 years of age.
Were there any differences in how well the drug worked in clinical trials among sex, race, and age groups?
The table below summarizes efficacy results by sex, race and age.
Table 3. Evaluation of mNIS+7 by Subgroup
|
Subgroup |
Baseline |
Change from Baseline at Week 66 LS Mean (SEM) |
TEGSEDI-Placebo Treatment Difference |
||
|---|---|---|---|---|---|
|
|
TEGSEDI |
Placebo |
TEGSEDI |
Placebo |
|
|
Sex |
|||||
|
Male |
75, 82 |
41, 79 |
6.1 (2.5) |
25.6 (3.2) |
-19.5 (-27.5, -11.5) |
|
Female |
31, 72 |
18, 64 |
5.1 (3.8) |
25.4 (5.0) |
-20.3 (-32.6, -8.0) |
|
Race |
|||||
|
White |
100, 81 |
53, 76 |
5.7 (2.2) |
24.3 (2.8) |
-18.6 (-25.5, -11.7) |
|
Other |
6, 57 |
6, 56 |
7.1 (10.9) |
37.0 (8.8) |
-29.8 (-57.2, -2.5) |
|
Age Group |
|||||
|
< 65 years |
59, 78 |
34, 70 |
5.7 (2.8) |
23.4 (3.6) |
-17.8 (-26.5, -9.0) |
|
> 65 years |
47, 81 |
25, 80 |
5.9 (3.2) |
28.2 (4.1) |
-22.3 (-32.5, -12.0) |
FDA Review
What are the possible side effects?
TEGSEDI can cause serious side effects, including low platelet counts and kidney inflammation. Because of these serious side effects, TEGSEDI is available only through a restricted program called the TEGSEDI Risk Evaluation and Mitigation (REMS) Program.
Other serious side effects include stroke, serious inflammatory and immune system problems, abnormal liver function, and decreased vitamin A levels.
The most common side effects are injection site reactions (redness, swelling, bleeding, pain, rash, and itching at the injection site), nausea, headache, tiredness, low platelet counts, and fever.
What are the possible side effects (results of trials used to assess safety)?
The table below summarizes adverse reactions in patients with hereditary transthyretin-mediated amyloidosis.
Table 4. Adverse Reactions Reported in At Least 5% TEGSEDI-Treated Patients and that Occurred At Least 5% More Frequently or At Least Two Times More Frequently than Placebo Patients
|
TEGSEDI |
Placebo |
|
|---|---|---|
|
Injection site reactionsa |
49 |
10 |
|
Nausea |
31 |
12 |
|
Headache |
26 |
12 |
|
Fatigue |
25 |
20 |
|
Thrombocytopenia |
24 |
2 |
|
Fever |
20 |
8 |
|
Peripheral edema |
19 |
10 |
|
Chills |
18 |
3 |
|
Anemia |
17 |
3 |
|
Vomiting |
15 |
5 |
|
Myalgia |
15 |
10 |
|
Decreased renal function |
14 |
5 |
|
Arrhythmiab |
13 |
5 |
|
Arthralgia |
13 |
8 |
|
Pre-syncope or syncope |
13 |
5 |
|
Decreased appetite |
10 |
0 |
|
Paresthesia |
10 |
3 |
|
Dyspnea |
9 |
3 |
|
Elevated liver function test |
9 |
3 |
|
Orthostasis |
8 |
2 |
|
Influenza like illness |
8 |
3 |
|
Contusion |
7 |
2 |
|
Bacterial infectionc |
7 |
3 |
|
Eosinophilia |
5 |
0 |
|
Dry mouth |
5 |
2 |
a Includes bruising, erythema, hematoma, hemorrhage, induration, inflammation, mass, edema, pain, pruritus, rash, swelling, and urticaria.
b Includes arrhythmia, atrial fibrillation, atrial flutter, bradyarrhythmia, bradycardia, extrasystoles, sinus arrhythmia, sinus bradycardia, supraventricular extrasystoles, tachycardia, and ventricular extrasystoles.
c Includes bacteremia, cellulitis staphylococcal, clostridium difficile infection, conjunctivitis bacterial, cystitis Escherichia, Helicobacter gastritis, Helicobacter infection, Staphylococcal infection.
TEGSEDI Prescribing Information
Were there any differences in side effects among sex, race and age?
- Sex: The occurrence of side effects was similar in males and females.
- Race: The majority of patients in the trial was White. Differences in the occurrence of side effects among races could not be determined because of the small number of patients in other races.
- Age: The occurrence of congestive heart failure, muscle and extremity pain, and chills was increased in patients 65 years of age and older.
Were there any differences in side effects of the clinical trials among sex, race, and age groups?
The table below summarizes the occurrence of the most common adverse reaction, injection site reactions, by subgroup.
Table 5. Subgroup Analysis of Injection Site Reactions
|
Demographic Characteristic |
TEGSEDI |
Placebo |
|---|---|---|
|
Sex |
||
|
Male |
39/77 (51) |
1/41 (2) |
|
Female |
16 /35 (46) |
5/19 (26) |
|
Race |
||
|
White |
52/105 (50) |
5/53 (9) |
|
Black or African American |
1/3 (33) |
0 /1 (0) |
|
Asian |
1/1 (100) |
0 /3 (0) |
|
Other |
1/3 (33) |
1 /3 (33) |
|
Age Group |
||
|
< 65 years |
34 /64 (53) |
3/34 (9) |
|
> 65 years |
21/48 (44) |
3/26 (12) |
Clinical Trial Data
Table 6. Adverse Reactions with At Least a 10% Difference Between Subgroups (in either Treatment Group) by Preferred Term and Age
|
TEGSEDI |
Placebo |
|||
|---|---|---|---|---|
|
|
< 65 years |
> 65 years |
< 65 years |
> 65 years |
|
Cardiac failure congestive |
0 (0) |
9 (13) |
1 (3) |
1 (4) |
|
Chills |
7 (11) |
13 (27) |
1 (3) |
1 (4) |
|
Peripheral Edema |
9 (14) |
12 (25) |
2 (6) |
4 (15) |
|
Decreased platelet count |
4 (6) |
8 (17) |
0 (0) |
0 (0) |
|
Myalgia |
6 (10) |
11 (23) |
5 (15) |
1 (4) |
|
Pain in Extremity |
3 (5) |
7 (15) |
7 (21) |
1 (4) |
Adapted from FDA Review
WHO WAS IN THE STUDIES?
Who participated in the clinical trials?
The FDA approved TEGSEDI based on evidence from one clinical trial (Trial 1/NCT01737398) that included 172 patients with hereditary transthyretin-mediated amyloidosis. The trial was conducted at 24 sites in Australia, Europe, South America, and the United States.
Figure 1 summarizes how many men and women were in the clinical trial.
Figure 1. Baseline Demographics by Sex
FDA Review
Figure 2 summarizes the percentage of patients by race in the clinical trial.
Figure 2. Baseline Demographics by Race
FDA Review
Teble 1. Demographics of Trial by Race
|
Race |
Number of Patients |
Percentage of Patients |
|---|---|---|
|
White |
158 |
93% |
|
Black or African American |
4 |
2% |
|
Asian |
4 |
2% |
|
Other |
5 |
3% |
FDA Review
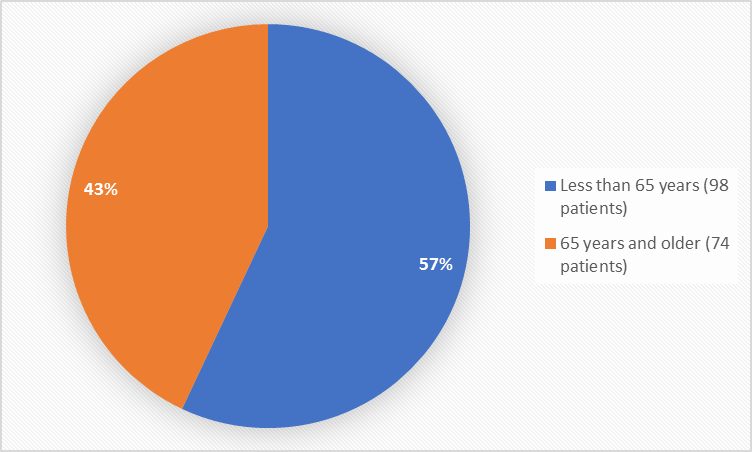
Figure 3 summarizes the percentage of patients by age in the clinical trial.
Figure 3. Baseline Demographics by Age
FDA Review
The table below summarizes demographics of all patients in the clinical trial.
Table 7. Demographic Characteristics
|
|
TEGSEDI |
Placebo |
TOTAL |
|---|---|---|---|
|
Sex, n (%) |
|||
|
Male |
77 (69) |
41 (68) |
118 (69) |
|
Female |
35 (31) |
19 (32) |
54 (31) |
|
Race, n (%) |
|||
|
White |
105 (94) |
53 (88) |
158 (92) |
|
Black or African American |
3 (3) |
1 (2) |
4 (2) |
|
Asian |
1 (< 1) |
3 (5) |
4 (2) |
|
Other |
3 (3) |
2(3) |
5 (3) |
|
Age (years) |
|||
|
Mean (SD) |
59.0 (12.5) |
59.5 (14.1) |
59.3 (13.3) |
|
Median |
62 |
63 |
63 |
|
Minimum, Maximum |
27, 78 |
28, 81 |
27, 81 |
|
Age Group, n (%) |
|||
|
Less than 65 years |
64 (57) |
34 (57) |
98 (57) |
|
65 years and older |
48 (43) |
26 (43) |
74 (43) |
|
Ethnicity, n (%) |
|
|
|
|
Hispanic |
17 (15) |
7 (12) |
24 (14) |
|
Non-Hispanic |
95 (85) |
53 (88) |
148 (86) |
|
Region, n (%) |
|
|
|
|
Europe |
37 (33) |
23 (38) |
60 (35) |
|
South America/Australia |
19 (17) |
11 (18) |
30 (17) |
|
United States |
56 (50) |
26 (43) |
82 (48) |
Clinical Trial Data
How were the trials designed?
The benefits and side effects of TEGSEDI were evaluated in one clinical trial that enrolled patients with hereditary transthyretin-mediated amyloidosis. Patients were randomly assigned to receive TEGSEDI or placebo by subcutaneous injection given once a week for 65 weeks. During the first week of treatment, patients received 3 doses of treatment, followed by once weekly subcutaneous injections for 64 weeks. Neither the patients nor the health care providers knew which treatment was being given until after the trial was completed.
Health care providers rated the change in the signs and symptoms of neuropathy (nerve damage) from baseline to Week 66 using a numerical scale. Changes from baseline to Week 66 in the impact of neuropathy on patients’ daily functioning were also evaluated using a numerical scale. The scores for the patients receiving TEGSEDI were compared to the scores for the patients receiving placebo.
How were the trials designed?
The efficacy and safety of TEGSEDI were established in one randomized, double-blind, placebo-controlled trial. The trial evaluated TEGSEDI for the treatment of polyneuropathy of hereditary transthyretin-mediated amyloidosis in adults. Patients were randomized to receive TEGSEDI or placebo as a subcutaneous injection administered for 65 weeks. Three doses were administered during the first week, followed by a subcutaneous injection once weekly for the remaining 64 weeks. The co-primary efficacy endpoints were the change from baseline to Week 66 in the modified Neuropathy Impairment Score +7 (mNIS+7) and the Norfolk Quality of Life Diabetic Neuropathy (QoL-DN) total score.
The mNIS+7 is an objective assessment of neuropathy that comprises the NIS and Modified +7 composite scores. The NIS measures deficits in cranial nerve function, muscle strength, reflexes, and sensation. The Modified +7 assesses heart rate response to deep breathing, postural blood pressure, quantitative sensory testing, and peripheral nerve electrophysiology. Health care providers rate severity on a maximum possible score of 346.32 points. Higher scores represent greater severity of disease. The clinical meaningfulness of the objective findings on the mNIS+7 was assessed by the change from baseline to Week 66in the Norfolk- Quality of Life-Diabetic Neuropathy (Norfolk-QoL-DN) score. The Norfolk-Qol-DN is a patient-reported assessment that evaluates physical function/large fiber neuropathy, activities of daily living, symptoms, small fiber neuropathy, and autonomic neuropathy. The maximum possible score was 136. Higher scores represent greater impairment.
GLOSSARY
CLINICAL TRIAL: Voluntary research studies conducted in people and designed to answer specific questions about the safety or effectiveness of drugs, vaccines, other therapies, or new ways of using existing treatments.
COMPARATOR: A previously available treatment or placebo used in clinical trials that is compared to the actual drug being tested.
EFFICACY: How well the drug achieves the desired response when it is taken as described in a controlled clinical setting, such as during a clinical trial.
PLACEBO: An inactive substance or “sugar pill” that looks the same as, and is given the same way as, an active drug or treatment being tested. The effects of the active drug or treatment are compared to the effects of the placebo.
SUBGROUP: A subset of the population studied in a clinical trial. Demographic subsets include sex, race, and age groups.
PRESCRIBING INFORMATION